Mediastinal giant parathyroid adenoma—a minimally invasive mediastinal surgical approach for an emergency presentation
Clinical vignette
A 72-year-old female was referred to our unit with a right sided hemothorax following biopsy of a paratracheal mass (Video 1).

The patient was initially seen by her general practitioner for hypertension. Routine blood investigations revealed hypercalcemia, (calcium 2.00 mmol/L, adjusted calcium 3.02 mmol/L) and hypophosphatemia (phosphate 0.84 mmol/L). Parathyroid hormone (PTH) levels were significantly raised at 26.6 mmol/L. The patient had a background history of depression but was otherwise asymptomatic and physical examination was unremarkable. She was referred to an endocrinologist and investigated for primary hyperparathyroidism. The patient was found to be osteoporotic on dual energy X-ray absorptiometry (DEXA) scanning (T score =−3.2 at the lumbar spine).
Neck ultrasound revealed an incidental thyroid nodule, but no obvious parathyroid lesion. A technetium sestamibi (99 mTc MIBI) scan showed no evidence of a parathyroid adenoma. Computed tomography (CT) revealed a complex cystic solid mass (Figure 1A) in the mediastinum, closely related to the right lateral aspect of the trachea, the esophagus, the superior vena cava (SVC) and the right subclavian artery and veins.
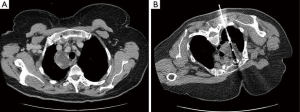
A CT-guided biopsy (Figure 1B) was performed following multidisciplinary discussion, confirming a parathyroid adenoma on histology. The patient developed a right sided apical pneumothorax following the biopsy which was managed with a chest drain, and she was discharged. She was readmitted after one week, with a 3-day history of progressive shortness of breath but was hemodynamically stable. A repeat CT scan showed a large right pleural effusion (Figure 2) with no active contrast extravasation.

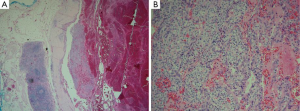
The patient underwent drainage of the hemothorax with excision of the adenoma via video assisted thoracoscopy (VATS). The mass was found to be actively bleeding intra-operatively. Histology identified it as a 19-g mediastinal giant parathyroid adenoma macroscopically, with a large hemorrhage-filled cavity and a thick, calcified wall (Figure 3) and microscopically (Figure 4) without evidence of malignancy.

Surgical technique
Preparation
The patient was intubated using a left-sided double lumen endotracheal tube under general anesthesia and placed in the left lateral decubitus position, with pressure care, standard skin preparation and draping. The right lung was deflated prior to the utility incision.
Exposition
A 4.5-cm utility incision was made in the right fifth intercostal space, anterior to latissimus dorsi muscle. Two additional 1.5 cm VATS incisions in the sixth and seventh intercostal space were made in the anterior and posterior axillary lines.
Operation
A total of 3.9 L of hemorrhagic fluid was evacuated from the right pleural cavity. The mediastinal mass was closely adjacent to the superior vena cava (SVC), the right innominate and subclavian veins as well as the subclavian artery, vagus nerve, recurrent laryngeal nerve and the trachea. The mediastinal pleura was incised inferiorly and along both sides of the mass using the Harmonic ACE +7 Laparoscopic Shears (Ethicon), with careful preservation of the tumor capsule. The tumor was freed at the lateral and inferior parts using blunt and sharp dissection. The superior part of the tumor was closely related to the large vessels. The parietal pleura at this level was challenging to access, as it had been obscured by the mass of the tumor. Traction was applied on the pleural coverage on the superior of the mass and direct traction on the mass was avoided to prevent rupture of the capsule and pleural dissemination. Traction on the pleural coverage enabled exposure of the superior aspect of the mass. It was gradually uncovered and the pleura on the superior aspect was incised completely. The remainder of the tissue, including the feeding vessels, was divided with the Harmonic scalpel. The resected tumour was then removed with a 10 cm Endo Catch bag (Covidien). Analgesia was administered in the form of a chirocaine intercostal block and paravertebral extrapleural catheter. A 28 French Portex chest drain (Smiths Medical) was inserted via the lower anterior incision and connected to a Thopaz Portable Suction System (Medela) on −1.5 kPa of suction.
Completion
Vicryl 1 was used for closure of the muscles and subcutaneous tissue, with Monocryl 3-0 for skin closure. The patient did not require a transfusion. Analgesia was administered in the form of a patient controlled morphine pump (50 mg in 50 mL 0.9% normal saline) and a ropivacaine paravertebral block (2 mg/mL).
Comments
Clinical results
The patient received routine post-operative care on a standard ward. Biochemical markers normalized immediately. The chest drain was removed and she was discharged on the third postoperative day.
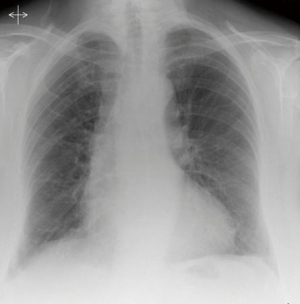
A chest radiograph at six weeks showed bilaterally well expanded lungs (Figure 5).
Follow up at eight weeks revealed normal calcium and PTH levels.
Vocal changes were noted immediately post-operatively, with hoarseness and a bovine cough. Although the recurrent laryngeal nerve was visualized intra-operatively and there was no obvious direct damage, these symptoms were suspicious of a recurrent laryngeal nerve injury. The patient’s voice normalized at eight weeks.
Advantages
Primary hyperparathyroidism is most commonly caused by parathyroid adenomas or hyperplasia. Parathyroid tumors larger than 2 g are considered to be “giant” parathyroid adenomas (1), with the largest documented to weigh 135 g (2). Mediastinal parathyroid adenomas are rare and are usually solitary (3). They can be successfully resected through a VATS approach, which minimizes the complications associated with sternotomy or thoracotomy. Radionucleotide-guided localization can be used intraoperatively, with injection of technetium (4). In our case, the pre-operative 99 mTc MIBI scans were negative and hence this technique was not appropriate. Moreover, this was a minimally invasive approach for an emergency presentation, with the large hemothorax as the primary indication for surgery. The tumor was successfully resected and biochemical markers normalized.
Caveats
Intra-operative PTH testing has been previously used to confirm parathyroid adenoma resection (5). An intra-operative fall of PTH levels of >50% was considered to indicate complete resection. Persistently elevated intra-operative levels were thought to warrant neck exploration. This method was not used in this case as this was an emergency presentation. Furthermore, the lesion was well circumscribed on pre-operative imaging and in vivo, with no evidence of extramediastinal ectopic tissue and normal post-operative biochemistry.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Meyer-Rochow G, Sidhu SB, Delbridge LW, et al. ES12 Can giant parathyroid adenomas be safely removed by minimally invasive parathyroidectomy? ANZ J Surg 2007;77:A23.
- Rubello D, Manente S, Casara D, et al. Clinically silent giant parathyroid adenoma: differential diagnosis and therapeutic approach. Clin Nucl Med 2003;28:519-21. [PubMed]
- Aggarwal V, Mishra A, Bhargav PR, et al. Giant parathyroid adenoma. ANZ J Surg 2009;79:91. [PubMed]
- Ott MC, Malthaner RA, Reid R. Intraoperative radioguided thoracoscopic removal of ectopic parathyroid adenoma. Ann Thorac Surg 2001;72:1758-60. [PubMed]
- O'Herrin JK, Weigel T, Wilson M, et al. Radioguided parathyroidectomy via VATS combined with intraoperative parathyroid hormone testing: the surgical approach of choice for patients with mediastinal parathyroid adenomas? J Bone Miner Res 2002;17:1368-71. [PubMed]





