Conditional long-term survival following minimally invasive robotic mitral valve repair: a health services perspective
Introduction
Mitral valve repair is the most common robotically assisted cardiac procedure currently performed, with many surgeons transitioning from traditional sternotomy to this approach (1,2). The procedure is usually indicated in patients with ischemic or myxomatous mitral valve prolapse and excessive leaflet motion (3). When the mitral valve does not close properly, blood shunts back into the left atrium and the pulmonary vessels, decreasing the movement of oxygen-rich blood from the heart to other vital organs of the body. Over time, the increasing severity of regurgitation may cause left atrial dilatation and pulmonary edema, eventually leading to congestive heart failure (HF). Symptoms associated with mitral valve disease include dyspnea, fatigue, palpitations, chest pain or syncope (4).
The robotically assisted, minimally invasive mitral valve repair procedure (RMVP) has several advantages over traditional repair (decreased perioperative blood loss, atrial fibrillation, sternal wound infections, hospital length of stay, and less invasive incisions) (5). RMVP is also associated with reduced length of recovery period postoperatively, more rapid return to normal activities of daily living, and fewer redo valvular interventions (1,5-9). However, it remains unclear whether these advantages translate into effective economic healthcare policy over the lifespan of the patient.
The selection of patients who would benefit from a robotically assisted procedure is a critical step in the preoperative planning stage. While the robotic approach is contraindicated in patients with certain anatomical and functional abnormalities, there is a paucity of data on risk factors associated with long-term survival in this population, especially those undergoing RMVP (1). Conditional survival, by accounting for time already survived after surgery, provides a more accurate measure of future survival than standard preoperative estimates (10). This paper aims to identify predictive factors that influence long-term conditional survival in patients who have undergone RMVP and to assign probabilities for survival in the form of a conditional risk-stratification matrix.
Patients and methods
This study has been approved by the institutional review board of Brody School of Medicine at East Carolina University. Details of data collection and management have been previously described and are briefly summarized below (2).
Study design
The study included 641 consecutive patients undergoing RMVP with annuloplasty band from May 2000 to April 2011 at East Carolina Heart Institute (ECHI). Demographic data, comorbid conditions, preoperative medication and surgical details were collected at the time of surgery. Racial identity was self-reported. Patients who presented with severely calcified mitral annulus, significant pulmonary hypertension (HTN) [pulmonary artery systolic pressure (PAS) >70 mmHg], or requiring aortic valve replacement were excluded.
Operative procedure
All procedures were performed at the ECHI using the da Vinci robotic surgical system (Intuitive Surgical, Inc, Sunnyvale, CA, USA). This minimally invasive system, approved by the U.S. Food and Drug Administration (FDA), uses telemanipulative controls that are actuated by the surgeon’s hand and finger movements, endoscopic camera visualization and endoscopic instrumentation. The procedure is performed through the right lateral thoracotomy approach with small port and access incision sites (7). Technical advances include three-dimensional visualization, tremor filtration and motion scaling to facilitate steady micro-movements (2).
Once anesthesia, echocardiographic assessment and robotic access were achieved, standard mitral repair techniques were used for both simple and complex reconstructions (2). Annular reduction was achieved in all patients using annuloplasty with either the Cosgrove-Edwards (Edwards Lifesciences, Inc., Irvine, CA, USA) or the ATS Simulus® (Medtronic, Inc., Minneapolis, MN, USA) band. Instrumentation of all leaflet resections and repairs, chordal reconstructions, band implantations, and suture knot tying were performed robotically using minimally invasive access. When appropriate, coronary artery bypass graft was performed concurrently with RMVP to manage left main coronary artery disease (LMCA) and three-vessel disease.
Definitions
Mitral insufficiency (MI) was defined as having non-ischemic degenerative type mechanical failure (usually the result of leaflet prolapse) of the mitral valve resulting in moderate to severe regurgitation as graded by echocardiography. Transesophageal echocardiography was used to grade MI both preoperatively and postoperatively. RMVP referred to any repair of MI using the Da Vinci® robotic surgical system at our institution followed by annuloplasty band placement. This included chordal procedures and leaflet resections. Operative mortality was defined as any cause of death within 30 days after mitral valve repair surgery in or out of our hospital and after 30 days during the same hospitalization following surgery.
Comorbidities such as chronic obstructive pulmonary disease (COPD), coronary artery disease (CAD), HF, HTN, diabetes (DM), LMCA, and peripheral vascular disease (PAD) were defined as having a preoperative diagnosis according to standard Society of Thoracic Surgeons (STS) definitions (11). This included physician documentation or other medical records (e.g., hospital notes, medication reports, outpatient medical records and radiology readings). Recent echocardiogram reports were reviewed for left ventricular ejection fractions (LVEF), and left ventricular dysfunction was defined as LVEF below 0.35. Patients with postoperative atrial fibrillation were those presenting with a first time episode lasting greater than 1 hour post-operatively and requiring treatment. Three-vessel coronary disease included stenosis of three different coronary arteries. Recent smoking status was defined as use of cigarettes within 1 year prior to surgery. This excluded cigars, pipes, chewing tobacco, dipping tobacco and snuff.
Setting
ECHI is a population-based tertiary heart hospital providing a full range of cardiovascular care services including cardiac surgery and cardiology to counties predominately located in the eastern region of North Carolina (12,13). The institute is the largest stand-alone cardiovascular care center in the state of North Carolina.
Data collection and follow up
Information was extracted from the STS Adult Cardiac Surgery Database at ECHI and the shared electronic health record (EHR) system at Vidant Medical Center and Brody School of Medicine. The consolidation of local and regional clinics throughout our system into a single EHR occurred in 2005, which has facilitated the efficient follow-up of patients undergoing surgery at ECHI. Quality checks and cross-field validation of data are routinely performed by the Center for Epidemiology and Outcomes Research at the Institute. These checks include a series of computerized logic algorithms to identify mismatching of patient data across clinics and follow-up visits.
The National Death Index (NDI), using social security numbers as the patient identifier, was employed to verify death information captured in our EHR and to ascertain death dates for patients lost to follow-up (14-16). The use of social security numbers was proscribed by our university in 2011 in accordance with §205(r) of the Social Security Act (17).
Statistical analysis
Categorical variables were reported as frequency and percentage, while continuous variables were reported as median and interquartile range. Patients were stratified by standard demographic variables (sex and age group) as previously described (10). Fisher’s exact test was used to determine statistical significance for categorical variables and the Kruskal-Wallis test for continuous variables. Given that a patient had already survived x years after surgery, conditional survival was defined as the probability of surviving an additional y years (18). The exponential Greenwood formula was used to compute variance for conditional survival, allowing for confidence intervals (CI) bounded by 0 and 1 (19). Hazard ratios (HR) and 95% CI for traditional survival models were computed using Cox proportional hazards regression.
Conditional survival models were adjusted for demographic and clinical variables using the multivariable product-limit method (19). This procedure is known to have strong uniform consistency and other desirable statistical properties (20-22). Model cross-validation and performance were assessed by computing the percentage difference of fitted probabilities under the multivariable product-limit model to observe probabilities measured nonparametrically using stratified Kaplan-Meier survival estimates (10). The percent differences within ±2.5% were considered to be in the equivalence zone and coded as zero. A Deuchler-Wilcoxon procedure was used to test the null hypothesis that the general measure of central tendency for the percentage differences did not differ from zero (23). The discriminate abilities of our models were assessed by computing the c-statistic concordance probability given censoring (24-26). An interaction of variables by time may affect the overall model fit and performance (parallel hazard assumption). A test for this assumption was performed by including time dependent covariates in our proportional-hazards regression models.
A conditional risk-stratification matrix was constructed, including (I) key demographic variables (age, sex) and (II) modifiable risk factors that were identified to be significantly associated with long-term survival in the traditional multivariable Cox regression model. Race was excluded from the matrix owing to limited sample size.
The Holly and Whittemore method was used for rounding (27). P<0.05 was defined as statistically significant. SAS Version 9.4 (Cary, NC, USA) was used for all analyses.
Results
A total of 641 patients (60% men, 34% >65 years of age) underwent RMVP with annuloplasty band during the study period (Table 1). HTN, atrial fibrillation and peripheral artery disease were more prevalent in patients greater than 65 years among both men and women (P≤0.0001). Similarly, those aged >65 years had increased use of lipid lowering agents, β-blockers and digitalis than patients ≤65 years (P<0.0001) (Table 2). There were no unexpected variations between age-sex groups for aortic cross-clamp, perfusion, intensive care unit and hospitalization time (Table 3). Procedural complication rates were low across groups with the exception of atrial fibrillation (n=157 cases). Operative mortality was higher among patients receiving RMVP with MAZE/Ablation (n=12) than patients receiving RMVP alone (n=1).
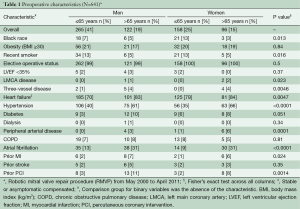
Full table
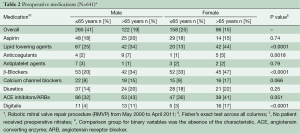
Full table
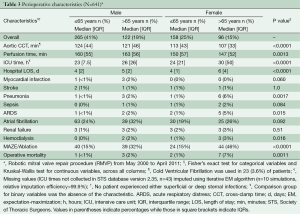
Full table
Among demographic factors (age, sex, race), only age >65 years was associated with decreased long-term survival (multivariable HR 6.9, 95% CI 3.3-15). Similarly, among modifiable risk factors (obesity, HTN, HF, COPD, DM, atrial fibrillation, recent smoking history), only atrial fibrillation (multivariable HR 2.1, 95% CI 1.1-4.0) and recent history of smoking (multivariable HR 3.0, 95% CI 1.2-7.5) were associated with decreased long-term survival (Table 4).
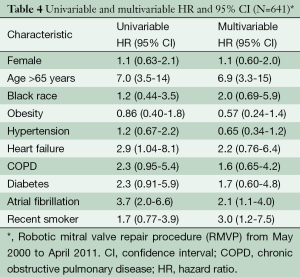
Full table
Our conditional risk-stratification matrix consisted of age, sex, recent smoking and preoperative cardiac rhythm (Table 5). Non-smoking men (≤65 years) who presented in sinus rhythm had a 99% and 96% survival probability at 5 and 10 years, respectively, after surviving the first year following RMVP. In contrast, recent male smokers (>65 years) with preoperative atrial fibrillation had a 61% and 14% conditional survival probability at 5 and 10 years, respectively. Similar results were seen for recent female smokers (>65 years) with preoperative atrial fibrillation (58% 5-year and 11% 10-year conditional survival probability).
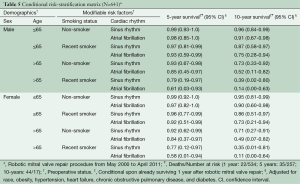
Full table
No serious violations of the proportional-hazards assumption were detected in our analyses. Percentage difference values for model variables were within the predefined equivalence region, indicating good model performance, while model discrimination exceeded chance.
Discussion
The number of isolated mitral valve repair procedures has increased exponentially from approximately 5,000 cases in 2005 to around 65,000 cases in 2014, with RMVP increasingly gaining favor among cardiothoracic surgeons (1,2,28). However, while robotic procedures are deemed just as safe as invasive open heart surgery, there is significant investment required for the installation and maintenance of robotic equipment, as well as the rigorous training of surgeons (29). Determining which patients would benefit the most from RMVP, especially in terms of cost and expected long-term survival, is an important component in the preoperative selection of patients with mitral valve insufficiency. Our study has provided useful information on predictive factors for long-term survival among patients who survived the initial one-year postoperative period following RMVP.
Assessing survival from the time of surgery can be misleading because the probability of survival is dynamic. This study used conditional methods, which provide a more accurate measure of future prognosis than standard methods for estimating long-term survival (18). We identified a parsimonious conditional risk-stratification matrix that included clinically relevant demographic variables (regardless of their importance in the current data set) and statistically significant modifiable risk factors. Amending the latter risk factors preoperatively can prove favorable for the patient’s long-term outcome, for example, cessation programs for smoking and medical management of atrial fibrillation (pharmacologic, cardioversion, ablation). This by no means advocates exposing the patient to the consequences of delayed intervention, especially when early repair is available, but rather making certain the patient is properly managed preoperatively to obtain the best long-term outcome (6,30).
Identifying candidates most suitable for RMVP will help to optimize patient outcomes and reduce procedural cost, currently exceeding $30,000 per case (31). This includes determining which patients ultimately will survive the longest in lieu of competing risks (concomitant comorbidities). The acceptance of RMVP also has benefited from several recent cost-saving innovations, such as the use of nitinol alloy U-clips and the novel Cor-Knot™ device (credited with reducing cardiopulmonary bypass and cross-clamp times) (32-34). Further intraoperative process improvements have been achieved through coordinated case sequencing across rooms, integrated staffing models and punctual operative start times (31). Although the initial capital investment in robotic technology remains high, this is offset by better postoperative quality of life and anticipated prolonged lifespan for patients (34).
Our findings have demonstrated that patients who are appropriately selected during the preoperative period have 5-year survival probabilities exceeding 90% for the majority of risk permutations (i.e., 10/16). Although certain subsets of patients, as highlighted in our analysis, are more likely to die in the long-term following the initial 1-year postoperative window, it must be emphasized that these deaths are likely attributed to the underlying force of mortality associated with comorbid conditions and patient age.
Operative mortality for RMVP in our study was fairly low (~2%). Among patients receiving isolated RMVP, there was only one recorded death. Patients receiving ablation (typically MAZE) along with RMVP accounted for the remaining operative deaths. MAZE is successful at restoring sinus rhythm and decreasing late stroke rates, however, both radiofrequency energy and cryoablation have known side effects that may potentially exacerbate life-threatening cardiovascular events (35). Radiofrequency ablation may result in acute thrombosis leading to myocardial ischemia or infarction, while cryoablation has been associated with intimal hyperplasia in late coronary stenosis. A known complication of MAZE is postoperative atrial fibrillation; however, it is unclear whether this complication merely reflects preoperative atrial fibrillation (~30%) in this predisposed mitral valve repair population (35-37). It should be noted that the benefits largely outweigh the risks in performing MAZE procedures (37,38).
This study is strengthened by its large, prospectively-maintained database of both men and women and long-term follow-up. The cohort was well-characterized with minimal missing data and the systematic collection of exposure and event information. Using both the EHR and NDI, we were able to reliably determine the death dates of the patients. However, the reason of death is not recorded in the NDI, and consequently, we cannot verify that the association between RMVP and long-term survival is non-causal in nature. The number of RMVP patients was reduced over time owing to patient death and those lost to follow-up. Accordingly, CI for conditional survival estimates may not be as precise for later time-point estimates.
A few additional limitations should be noted when interpreting these findings. While the analysis considered several potential confounding variables, unmeasured factors could have influenced study results, given its non-randomized nature. Education, income and socioeconomic positions were not available, and procedural complications, medications and other time-dependent variables were not included in the models because of their potential to be in the causal pathway. The data was collected from a single hospital system and may not be generalizable to other institutions performing this procedure. Nonetheless, our surgical performance results for RMVP (cross-clamp time, hospital length of stay, operative mortality, and 5-year postoperative survival) compare favorably with other high-volume, specialized centers (5,39).
Our recent smoker variable did not include the use of smokeless tobacco, which can have almost twice the nicotine level of cigarette smoking (40). Nicotine causes the release of catecholamines leading to increased blood pressure, changes in heart rate, cardiac arrhythmias and endothelial damage (40,41). Furthermore, information on pack years of smoking was not available. While the potential underestimation of nicotine use may have biased results, such bias likely would have been towards the null. We also cannot rule out bias owing to our simplistic definition of preoperative atrial fibrillation. For example, the atrial fibrillation episodes in our analysis were not classified as lasting less than seven days, more than seven days or ongoing long-term. While this data would have been informative, the additional stratification would have required a much larger sample size than currently available.
The multivariable product-limit method has several limitations inherent to modeling censored survival data using semi-parametric methods and must be considered when applying this technique. However, our resulting model did not deviate from the underlying parallel hazard assumption, and the log cumulative hazard for model covariates was approximately linear. Furthermore, there was no indication that censoring was related to the probability of a death occurring. The method that we used applied the hazard for an average individual rather than the mean survival estimated for a heterogeneous set of individuals (42,43). While this may have slightly affected adjusted estimates, the relative position of the risk permutations in our model was invariant with respect to either method. It should also be noted that the technique described in the manuscript is one that is commonly available in standard statistical software.
Conclusions
Our conditional survival results, by accounting for time already survived, provide a more accurate measure of future survival than traditional estimates computed at the time of surgery.
Future studies are needed to better understand and translate our results into improving the clinical management of patients, optimizing hospital resources and individualizing patient assessment.
Acknowledgments
We thank the East Carolina Heart Institute and the College of Nursing for providing valuable support to conduct this research.
Footnote
Conflicts of Interest: This manuscript has not been submitted or published elsewhere. The authors report no relationships with companies that may have a financial interest in the information contained in the manuscript.
References
- Bush B, Nifong LW, Alwair H, et al. Robotic mitral valve surgery-current status and future directions. Ann Cardiothorac Surg 2013;2:814-7. [PubMed]
- Nifong LW, Rodriguez E, Chitwood WR Jr. 540 consecutive robotic mitral valve repairs including concomitant atrial fibrillation cryoablation. Ann Thorac Surg 2012;94:38-42; discussion 43. [PubMed]
- Bonow RO, Carabello BA, Chatterjee K, et al. 2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease). Endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol 2008;52:e1-142. [PubMed]
- Harris C, Croce B, Harris R. Minimally invasive mitral valve surgery. Ann Cardiothorac Surg 2015;4:304. [PubMed]
- Cheng DC, Martin J, Lal A, et al. Minimally invasive versus conventional open mitral valve surgery: a meta-analysis and systematic review. Innovations (Phila) 2011;6:84-103. [PubMed]
- Suri RM, Antiel RM, Burkhart HM, et al. Quality of life after early mitral valve repair using conventional and robotic approaches. Ann Thorac Surg 2012;93:761-9. [PubMed]
- Mandal K, Alwair H, Nifong WL, et al. Robotically assisted minimally invasive mitral valve surgery. J Thorac Dis 2013;5 Suppl 6:S694-703. [PubMed]
- Woo YJ, Nacke EA. Robotic minimally invasive mitral valve reconstruction yields less blood product transfusion and shorter length of stay. Surgery 2006;140:263-7. [PubMed]
- Mihaljevic T, Jarrett CM, Gillinov AM, et al. Robotic repair of posterior mitral valve prolapse versus conventional approaches: potential realized. J Thorac Cardiovasc Surg 2011;141:72-80.e1-4.
- Efird JT, O'Neal WT, Camargo GA, et al. Conditional survival of heart failure patients after coronary artery bypass grafting. J Cardiovasc Med (Hagerstown) 2014;15:498-503. [PubMed]
- The Society of Thoracic Surgeons National Database. 2014 [cited 2015 3/27/2015]; Available online: .www.sts.org/national-database
- Efird JT, O'Neal WT, Anderson CA, et al. The effect of race and chronic obstructive pulmonary disease on long-term survival after coronary artery bypass grafting. Front Public Health Serv Syst Res 2013;1:00004. [PubMed]
- Efird JT, O'Neal WT, Gouge CA, et al. Implications of Hemodialysis in Patients Undergoing Coronary Artery Bypass Grafting. Int J Cardiovasc Res 2013;2:1000154. [PubMed]
- Welke KF, Ferguson TB Jr, Coombs LP, et al. Validity of the Society of Thoracic Surgeons National Adult Cardiac Surgery Database. Ann Thorac Surg 2004;77:1137-9. [PubMed]
- Lash TL, Silliman RA. A comparison of the National Death Index and Social Security Administration databases to ascertain vital status. Epidemiology 2001;12:259-61. [PubMed]
- Morales DL, McClellan AJ, Jacobs JP. Empowering a database with national long-term data about mortality: the use of national death registries. Cardiol Young 2008;18 Suppl 2:188-95. [PubMed]
- da Graca B, Filardo G, Nicewander D. Consequences for healthcare quality and research of the exclusion of records from the Death Master File. Circ Cardiovasc Qual Outcomes 2013;6:124-8. [PubMed]
- Henson DE, Ries LA. On the estimation of survival. Semin Surg Oncol 1994;10:2-6. [PubMed]
- Kalbfleisch JD, Prentice RL. The statistical analysis of failure time data. 2nd ed. John Wiley & Sons Inc., Hoboken, New Jersey, 2002.
- Csörgő S, Horváth L. The rate of strong uniform consistency for the product-limit estimator. Zeitschrift für Wahrscheinlichkeitstheorie und Verwandte Gebiete 1983;62:411-26.
- Horváth L. The rate of strong uniform consistency for the multivariate product-limit estimator. J Multivar Anal 1983;13:202-9.
- Bakry D. Lectures on probability theory: Ecole d'été de probabilitiés de Saint-Flour XXII, 1992. Gill RD, Molchanov SA, Bernard P, eds. Berlin: Springer-Verlag, 1994.
- Wittkowski KM, Song T. Nonparametric methods for molecular biology. Methods Mol Biol 2010;620:105-53. [PubMed]
- Altman DG. Prognostic models: a methodological framework and review of models for breast cancer. Cancer Invest 2009;27:235-43. [PubMed]
- Harrell Jr, Frank E. Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. New York: Springer, 2001.
- Pencina MJ, D'Agostino RB. Overall C as a measure of discrimination in survival analysis: model specific population value and confidence interval estimation. Stat Med 2004;23:2109-23. [PubMed]
- Holly EA, Whittemore AS, Aston DA, et al. Anal cancer incidence: genital warts, anal fissure or fistula, hemorrhoids, and smoking. J Natl Cancer Inst 1989;81:1726-31. [PubMed]
- Grover FL, Shahian DM, Clark RE, et al. The STS National Database. Ann Thorac Surg 2014;97:S48-54. [PubMed]
- Athanasiou T, Ashrafian H, Rowland SP, et al. Robotic cardiac surgery: advanced minimally invasive technology hindered by barriers to adoption. Future Cardiol 2011;7:511-22. [PubMed]
- Goldstone AB, Patrick WL, Cohen JE, et al. Early surgical intervention or watchful waiting for the management of asymptomatic mitral regurgitation: a systematic review and meta-analysis. Ann Cardiothorac Surg 2015;4:220-9. [PubMed]
- Suri RM, Thompson JE, Burkhart HM, et al. Improving affordability through innovation in the surgical treatment of mitral valve disease. Mayo Clin Proc 2013;88:1075-84. [PubMed]
- Smith JM, Stein H. Endoscopic placement of multiple artificial chordae with robotic assistance and nitinol clip fixation. J Thorac Cardiovasc Surg 2008;135:610-4. [PubMed]
- Nifong LW, Alwair H, Parker D, et al. Significant Reduction in Operative Times Using Cor-Knot in Robot-Assisted Mitral Valve Repair. Prague, Czech Republic, 2013.
- Seco M, Cao C, Modi P, et al. Systematic review of robotic minimally invasive mitral valve surgery. Ann Cardiothorac Surg 2013;2:704-16. [PubMed]
- Lawrance CP, Henn MC, Damiano RJ Jr. Concomitant Cox-Maze IV techniques during mitral valve surgery. Ann Cardiothorac Surg 2015;4:483-6.
- Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA 2001;285:2370-5. [PubMed]
- Ad N, Holmes SD, Pritchard G, et al. Association of operative risk with the outcome of concomitant Cox Maze procedure: a comparison of results across risk groups. J Thorac Cardiovasc Surg 2014;148:3027-33. [PubMed]
- Garcia-Villarreal OA. Minimally invasive full biatrial Cox maze IV: we are going in the right direction. J Thorac Cardiovasc Surg 2014;148:2442. [PubMed]
- Modi P, Hassan A, Chitwood WR Jr. Minimally invasive mitral valve surgery: a systematic review and meta-analysis. Eur J Cardiothorac Surg 2008;34:943-52. [PubMed]
- Chagué F, Guenancia C, Gudjoncik A, et al. Smokeless tobacco, sport and the heart. Arch Cardiovasc Dis 2015;108:75-83. [PubMed]
- Asplund K. Smokeless tobacco and cardiovascular disease. Prog Cardiovasc Dis 2003;45:383-94. [PubMed]
- Nieto FJ, Coresh J. Adjusting survival curves for confounders: a review and a new method. Am J Epidemiol 1996;143:1059-68. [PubMed]
- Ghali WA, Quan H, Brant R, et al. Comparison of 2 methods for calculating adjusted survival curves from proportional hazards models. JAMA 2001;286:1494-7. [PubMed]





