A meta-analysis of mitral valve repair versus replacement for ischemic mitral regurgitation
Introduction
Ischemic mitral regurgitation (IMR) is a frequent complication of myocardial infarction, occurring in 13% to 50% of cases (1,2). The presence of IMR portends a poor prognosis and is associated with reduced long-term survival and impaired functional status (2,3). The pathophysiology of IMR mainly relates to the chronic adverse left ventricular (LV) remodeling that occurs following myocardial injury resulting in tethered mitral leaflets with poor coaptation.
Current practice guidelines recommend mitral valve repair (MVr) or mitral valve replacement (MVR) for severe IMR, but do not specify which procedure represents the optimal surgical approach (4,5). Potential benefits of MVr over MVR have been well described for other etiologies of mitral valve disease, particularly degenerative MR (6). However, IMR poses a unique surgical challenge as mitral regurgitation (MR) can occur in the presence of a structurally normal valve. Given the lack of multiple prospective randomized trials, a rigorous assessment of MVr and MVR requires a systematic and critical analysis of the current literature. The present meta-analysis aimed to assess the clinical outcomes of patients who underwent MVr or MVR for IMR.
Methods
Search strategy and study selection
Electronic searches were performed using Ovid Medline, Embase, Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, Cochrane Methodology Register, Database of Abstracts of Reviews of Effects and ACP Journal Club from their dates of inception to July 2015. The search terms “mitral” and (“ischemic” or “ischaemic”) and (“repair” or “replacement” or “annuloplasty”) and (“mortality” or “death” or “survival”) were entered as keywords and MeSH terms. This was supplemented by hand searching the reference lists of key reviews and all potentially relevant studies.
Two reviewers (A.S. and D.D.) independently screened the title and abstract of records identified in the search. Full-text publications were subsequently reviewed separately if either reviewer considered the manuscript as being potentially eligible. Disagreements regarding final study inclusion were resolved by discussion and consensus.
Eligibility criteria
Eligible studies were those reporting peri-operative or late mortality following MVr and MVR in patients with IMR. Studies were excluded if: (I) cohorts had mixed mitral valve etiologies and mortality data for the ischemic subset could not be separately determined; (II) concomitant surgical ventricular restoration was performed in either group; (III) there were fewer than ten patients in either the MVr or MVR group.
All publications were limited to those involving human subjects and written in English. Abstracts, conference presentations, editorials and expert opinions were excluded. Review articles were omitted because of potential publication bias and duplication of results. When institutions published duplicated studies with accumulating numbers of patients or increased lengths of follow-up, only the most complete reports were included for quantitative assessment.
Data extraction
All data were independently extracted from text, tables and figures by two investigators (A.S. and D.D.). The final results were reviewed by the senior reviewer (C.C.). The pre-determined primary endpoints were peri-operative and late mortality. Peri-operative mortality was defined as death within 30 days after surgery or during the same hospitalization. Late mortality was defined as death occurring during study follow-up period (minimum 12 months). Secondary outcomes included recurrence of at least moderate MR (grade ≥2), mitral valve re-operation, and echocardiographic measurements of LV remodeling.
Statistical analysis
Baseline characteristics and operative details were presented as raw values (%), mean ± standard deviation or median [interquartile range (IQR)] unless otherwise indicated. Pooled values for clinical outcomes were calculated using the DerSimonian-Laird random-effects model (7). The relative risk (RR) was used as the summary statistic, and reported with 95% confidence intervals (CI). Meta-analyses were performed using random-effects models to take into account the anticipated clinical and methodological diversity between studies. The I2 statistic was used to estimate the percentage of total variation across studies due to heterogeneity rather than chance, with values exceeding 50% indicative of considerable heterogeneity.
Publication bias was assessed using funnel plots comparing log risk estimates with their standard error. Egger’s linear regression method and Begg’s rank correlation test were used to detect funnel plot asymmetry, and the Trim-and-Fill method was used to explore the impact of studies potentially missing due to publication bias (8-10). Statistical analysis was conducted with Review Manager Version 5.1.2 (Cochrane Collaboration, Software Update, Oxford, UK) and Comprehensive Meta-Analysis v2.2 (Biostat Inc, Englewood, NJ, USA). All P values were two sided, and values <0.05 were considered statistically significant.
Results
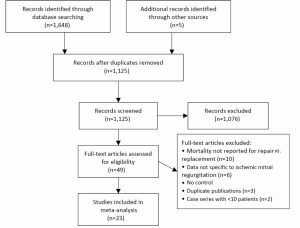
A total of 1,125 unique records were identified through the database searches. Of these, 1,076 were excluded on the basis of title and abstract content. After screening the full text of the remaining 49 articles, 23 studies met the criteria for inclusion (11-33). The study selection process is summarized in Figure 1.
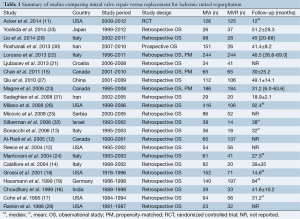
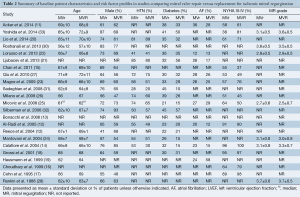
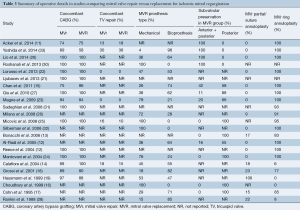
Of the included studies, there were 21 retrospective observational studies, one prospective observational study (OS) and one randomized controlled trial (Table 1). These included data on a total of 4,066 patients, including 2,357 patients who underwent MVr and 1,709 who underwent MVR. The median study sample size was 130 (range, 49-522). The mean or median follow-up duration was reported in 18 studies, ranging from 12 to 92.4 months. Baseline patient characteristics and risk factor profiles are summarized in Table 2, and a summary of operative details is presented in Table 3.
Full table
Full table
Full table
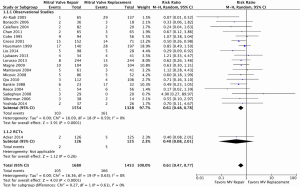
Peri-operative mortality
In 19 observational studies and one RCT involving a total of 3,133 patients, MVr was associated with significantly reduced perioperative mortality (pooled incidences of 6.6% vs. 11.4%; RR, 0.61; 95% CI, 0.47-0.77; I2=0%; P<0.001; Figure 2).
Late mortality
In ten observational studies and one RCT involving a total of 2,216 patients, MVr was associated with significantly reduced late mortality (pooled incidences of 16.8% vs. 22.2%; RR, 0.78; 95% CI, 0.67-0.92; I2=0%; P=0.002; Figure 3). The median lengths of follow-up of these studies ranged from 12 to 92.4 months.
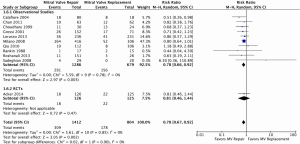
Subgroup analysis of late mortality was performed by duration of study follow-up. In studies with median follow-up ranging from 12-36 months, late mortality was not significantly reduced following MVr (pooled incidences of 15.7% vs. 19.4%; RR, 0.80; 95% CI, 0.56-1.13; I2=0%; P=0.20). In studies with median follow-up beyond 36 months, late mortality was significantly reduced following MVr (pooled incidences of 18.9% vs. 26.7%; RR, 0.78; 95% CI, 0.66-0.93; I2=0%; P=0.006).
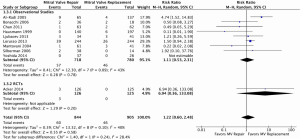
Mitral valve re-operation
At latest follow-up, MVr was not statistically significantly associated with mitral valve re-operation when compared to MVR using data from nine observational studies and one RCT involving a total of 1,749 patients (pooled incidences of 5.0% vs. 5.0%; RR, 1.22; 95% CI, 0.60-2.48; I2=40%; P=0.58; Figure 4).
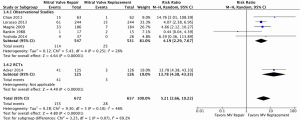
Recurrence of MR
At latest follow-up, recurrence of at least moderate MR was significantly higher following MVr in five observational studies and one RCT involving a total of 1,329 patients (pooled incidences of 22.1% vs. 4.5%; RR, 5.21; 95% CI, 2.66-10.22; I2=46%; P<0.001; Figure 5).
Echocardiographic measurements
A complete summary of pre- and post-operative echocardiographic measurements is displayed in Table S1. Due to the lack of raw data available, it was not possible to conduct meta-analyses for these endpoints.
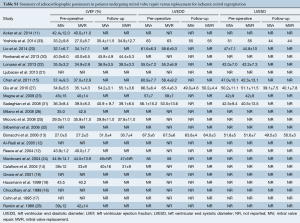
Full table
Sensitivity analyses
It was noted that earlier studies on MVr were associated with lower incidences of subvalvular preservation and use of annuloplasty ring, as shown in Table 3. Hence, sensitivity analyses were conducted to only include studies in which the mid-point of the study period was 2000 or later. Restricting analyses to these studies did not significantly impact on the result for peri-operative mortality (RR, 0.62; 95% CI, 0.42-0.91; I2=0%; P=0.01), late mortality (RR, 0.83; 95% CI, 0.70-0.90; I2=0%; P=0.04) or recurrence of at least moderate MR (RR, 5.64; 95% CI, 3.41-9.34; I2=20%; P<0.001). However, there was a trend towards increased mitral valve re-operation following MVr (RR, 1.47; 95% CI, 0.95-2.26; I2=0%; P=0.08).
Publication bias
Neither Begg’s rank correlation test (P=0.40) nor Egger’s linear regression method (P=0.29) suggested publication bias was a significant factor when peri-operative mortality was selected as an endpoint (Figure S1). Likewise, publication bias was not found to significantly influence results for late mortality (Begg’s rank correlation test, P=0.82; Egger’s linear regression method, P=0.89).

Discussion
In recent years, MVr has been increasingly performed in the surgical management of IMR (34). The Society of Thoracic Surgeons database from 2008-2012 reported that valve repair occurred in almost two-thirds of mitral valve surgeries in patients who underwent concurrent coronary artery bypass graft surgery (11). However, this trend of increased MVr has not been based on any conclusive evidence demonstrating superior outcomes for this approach.
To date, there has only been one RCT that has assessed clinical outcomes following MVr or MVR in patients with IMR. This RCT demonstrated similar 30-day and 12-month mortality between the two approaches (11). In contrast, our meta-analysis demonstrated significantly reduced peri-operative and late mortality in patients who underwent MVr. There are several possible reasons for this discrepancy. In clinical practice, high-risk patients with multiple co-morbidities and poor baseline function are often preferentially allocated to MVR over MVr. This was demonstrated by the patient characteristics of several included observational studies, in which patients within the MVR cohorts had significantly higher prevalence of baseline co-morbidities (Table 2) (19,33). Although several observational studies presented data for propensity-matched cohorts, these statistical methods are not a substitute for randomization, and key clinical confounders may have been omitted (35). It should also be noted that the only RCT to date had a relatively small sample size and follow-up was limited to 12 months. In the present meta-analysis, subgroup analysis demonstrated the reduction in late mortality following MVr to be most evident beyond 36 months, suggesting trials with shorter follow-up duration may be unable to detect potential mortality differences.
Both the randomized and observational data demonstrated a significantly higher rate of at least moderate MR following MVr (Figure 3). This represented an important finding as recurrence of MR >2 has been shown to be an independent predictor of poor long-term outcomes (36). Interestingly, the higher rate of recurrent MR did not translate to an increased incidence of mitral valve re-operation.
Several studies included in the present meta-analysis reported outdated surgical techniques, such as low rates of annuloplasty ring implantation with mitral repair (14,16,19,28). To account for this and ensure our results were relevant to contemporary surgical practice, we conducted sensitivity analyses excluding studies in which patients were mostly operated prior to 2000. These analyses did not significantly change the overall results obtained for peri-operative mortality, late mortality or recurrence of MR. However, in sensitivity analysis, there was a trend towards significantly higher rates of mitral valve re-operation following MVr. Of note, earlier studies tended to report lower preservation of both anterior and posterior leaflets during MVR (16,17). Bi-leaflet preservation has been shown to provide the greatest reduction in LV chamber size and systolic afterload, as well as maximal improvement in ventricular performance, and this may have contributed to a temporal effect on re-operation rates (37,38).
The findings of the present meta-analysis were limited by several key constraints. Firstly, the vast majority of included studies were single-center retrospective observational reports and thus had biases inherent to such study designs. Secondly, pre-operative and follow-up echocardiographic measurements were not reported in sufficient detail to enable meta-analysis, and could only be qualitatively summarized. This was a significant limitation as improvements in measurements such as LV volume index are significantly associated with improved clinical outcomes (39,40). Thirdly, quality of life endpoints and measures of functional status were also scarcely reported and thus could not be statistically analyzed in the present meta-analysis. Finally, follow-up periods and protocols differed widely between institutions and some studies may have reported lower rates of MR recurrence or mitral valve re-operation due to incomplete follow-up. However, in studies with specified follow-up periods, the minimum duration was 12 months.
In conclusion, the present meta-analysis demonstrated significantly reduced peri-operative and late mortality following repair versus replacement for patients with ischemic mitral valve regurgitation. However, these findings should be considered within the context of the clinical variables driving patient selection for each approach. Recurrence of at least moderate MR was significantly higher following MVr but rates of mitral valve re-operation were not significantly different. Larger studies with longer follow-up duration are required to further assess overall survival and freedom from re-intervention, as well as the impact of both surgical approaches on quality of life and functional status.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Hickey MS, Smith LR, Muhlbaier LH, et al. Current prognosis of ischemic mitral regurgitation. Implications for future management. Circulation 1988;78:I51-9. [PubMed]
- Bursi F, Enriquez-Sarano M, Jacobsen SJ, et al. Mitral regurgitation after myocardial infarction: a review. Am J Med 2006;119:103-12. [PubMed]
- Grigioni F, Enriquez-Sarano M, Zehr KJ, et al. Ischemic mitral regurgitation: long-term outcome and prognostic implications with quantitative Doppler assessment. Circulation 2001;103:1759-64. [PubMed]
- Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129:2440-92. [PubMed]
- Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC). Guidelines on the management of valvular heart disease (version 2012). Eur Heart J 2012;33:2451-96. [PubMed]
- Shuhaiber J, Anderson RJ. Meta-analysis of clinical outcomes following surgical mitral valve repair or replacement. Eur J Cardiothorac Surg 2007;31:267-75. [PubMed]
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. [PubMed]
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088-101. [PubMed]
- Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000;56:455-63. [PubMed]
- Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-34. [PubMed]
- Acker MA, Parides MK, Perrault LP, et al. Mitral-valve repair versus replacement for severe ischemic mitral regurgitation. N Engl J Med 2014;370:23-32. [PubMed]
- Al-Radi OO, Austin PC, Tu JV, et al. Mitral repair versus replacement for ischemic mitral regurgitation. Ann Thorac Surg 2005;79:1260-7; discussion 1260-7. [PubMed]
- Bonacchi M, Prifti E, Maiani M, et al. Mitral valve surgery simultaneous to coronary revascularization in patients with end-stage ischemic cardiomyopathy. Heart Vessels 2006;21:20-7. [PubMed]
- Calafiore AM, Di Mauro M, Gallina S, et al. Mitral valve surgery for chronic ischemic mitral regurgitation. Ann Thorac Surg 2004;77:1989-97. [PubMed]
- Chan V, Ruel M, Mesana TG. Mitral valve replacement is a viable alternative to mitral valve repair for ischemic mitral regurgitation: a case-matched study. Ann Thorac Surg 2011;92:1358-65; discussion 1365-6. [PubMed]
- Choudhary SK, Bhan A, Sharma R, et al. Post-infarction ischaemic mitral regurgitation: what determines the outcome. Indian Heart J 1999;51:508-14. [PubMed]
- Cohn LH, Rizzo RJ, Adams DH, et al. The effect of pathophysiology on the surgical treatment of ischemic mitral regurgitation: operative and late risks of repair versus replacement. Eur J Cardiothorac Surg 1995;9:568-74. [PubMed]
- Grossi EA, Goldberg JD, LaPietra A, et al. Ischemic mitral valve reconstruction and replacement: comparison of long-term survival and complications. J Thorac Cardiovasc Surg 2001;122:1107-24. [PubMed]
- Hausmann H, Siniawski H, Hetzer R. Mitral valve reconstruction and replacement for ischemic mitral insufficiency: seven years' follow up. J Heart Valve Dis 1999;8:536-42. [PubMed]
- Lio A, Miceli A, Varone E, et al. Mitral valve repair versus replacement in patients with ischaemic mitral regurgitation and depressed ejection fraction: risk factors for early and mid-term mortality†. Interact Cardiovasc Thorac Surg 2014;19:64-9. [PubMed]
- Ljubacev A, Medved I, Ostrik M, et al. Mitral regurgitation and coronary artery bypass surgery: comparison of mitral valve repair and replacement. Acta Chir Belg 2013;113:187-91. [PubMed]
- Lorusso R, Gelsomino S, Vizzardi E, et al. Mitral valve repair or replacement for ischemic mitral regurgitation? The Italian Study on the Treatment of Ischemic Mitral Regurgitation (ISTIMIR). J Thorac Cardiovasc Surg 2013;145:128-39; discussion 137-8. [PubMed]
- Magne J, Girerd N, Sénéchal M, et al. Mitral repair versus replacement for ischemic mitral regurgitation: comparison of short-term and long-term survival. Circulation 2009;120:S104-11. [PubMed]
- Mantovani V, Mariscalco G, Leva C, et al. Long-term results of the surgical treatment of chronic ischemic mitral regurgitation: comparison of repair and prosthetic replacement. J Heart Valve Dis 2004;13:421-8; discussion 428-9. [PubMed]
- Micovic S, Milacic P, Otasevic P, et al. Comparison of valve annuloplasty and replacement for ischemic mitral valve incompetence. Heart Surg Forum 2008;11:E340-5. [PubMed]
- Milano CA, Daneshmand MA, Rankin JS, et al. Survival prognosis and surgical management of ischemic mitral regurgitation. Ann Thorac Surg 2008;86:735-44. [PubMed]
- Qiu Z, Chen X, Xu M, et al. Is mitral valve repair superior to replacement for chronic ischemic mitral regurgitation with left ventricular dysfunction? J Cardiothorac Surg 2010;5:107. [PubMed]
- Rankin JS, Feneley MP, Hickey MS, et al. A clinical comparison of mitral valve repair versus valve replacement in ischemic mitral regurgitation. J Thorac Cardiovasc Surg 1988;95:165-77. [PubMed]
- Reece TB, Tribble CG, Ellman PI, et al. Mitral repair is superior to replacement when associated with coronary artery disease. Ann Surg 2004;239:671-5; discussion 675-7. [PubMed]
- Roshanali F, Vedadian A, Shoar S, et al. When to Repair Ischemic Mitral Valve Regurgitation: An Algorithmic approach. European Surgery 2013;45:98-105.
- Sadeghian H, Karimi A, Mahmoodian M, et al. Repair versus replacement for ischemic mitral regurgitation. Journal of Tehran University Heart Center 2008;2:89-94.
- Silberman S, Oren A, Klutstein MW, et al. Does mitral valve intervention have an impact on late survival in ischemic cardiomyopathy? IMAJ 2006;8:17-20. [PubMed]
- Yoshida K, Okada K, Miyahara S, et al. Mitral valve replacement versus annuloplasty for treating severe functional mitral regurgitation. Gen Thorac Cardiovasc Surg 2014;62:38-47. [PubMed]
- Gammie JS, Sheng S, Griffith BP, et al. Trends in mitral valve surgery in the United States: results from the Society of Thoracic Surgeons Adult Cardiac Surgery Database. Ann Thorac Surg 2009;87:1431-7; discussion 1437-9. [PubMed]
- Weitzen S, Lapane KL, Toledano AY, et al. Weaknesses of goodness-of-fit tests for evaluating propensity score models: the case of the omitted confounder. Pharmacoepidemiol Drug Saf 2005;14:227-38. [PubMed]
- Crabtree TD, Bailey MS, Moon MR, et al. Recurrent mitral regurgitation and risk factors for early and late mortality after mitral valve repair for functional ischemic mitral regurgitation. Ann Thorac Surg 2008;85:1537-42; discussion 1542-3. [PubMed]
- Yun KL, Sintek CF, Miller DC, et al. Randomized trial comparing partial versus complete chordal-sparing mitral valve replacement: effects on left ventricular volume and function. J Thorac Cardiovasc Surg 2002;123:707-14. [PubMed]
- Yun KL, Sintek CF, Miller DC, et al. Randomized trial of partial versus complete chordal preservation methods of mitral valve replacement: A preliminary report. Circulation 1999;100:II90-4. [PubMed]
- Di Donato M, Castelvecchio S, Menicanti L. End-systolic volume following surgical ventricular reconstruction impacts survival in patients with ischaemic dilated cardiomyopathy. Eur J Heart Fail 2010;12:375-81. [PubMed]
- Solomon SD, Skali H, Anavekar NS, et al. Changes in ventricular size and function in patients treated with valsartan, captopril, or both after myocardial infarction. Circulation 2005;111:3411-9. [PubMed]





