Minimally invasive primary aortic valve surgery: the OLV Aalst experience
Introduction
Minimally invasive aortic valve surgery (MI-AVS) is now widely performed (1,2) and it appears that there is a gradual shift in the literature from comparing outcomes with conventional surgery, towards determining which of the various MI-AVS approaches are most beneficial in terms of clinical outcome and patient satisfaction (3-8).
We initiated our MI-AVS program in October 1997, shortly after the first description and pioneering study by Cosgrove and Sabik (9). We elected to establish partial upper J-sternotomy aortic valve surgery (JS-AVS) as our preferred and routine approach for isolated AVS. We reported our findings on the benefits of this technique compared with conventional surgery (10) and demonstrated the feasibility of this approach in more complex cases involving the aortic root and ascending aorta (11) as well as redo-operation modality (12).
This study provides an in-depth overview of our minimally invasive JS-AVS experience in 768 patients who underwent isolated primary aortic valve procedures over a 16-year period.
Methods
This is a retrospective review of a single-center prospective database. A total of 768 patients underwent primary isolated JS-AVS (excluding redo-, aortic root- and ascending aorta procedures) between 1 October 1997 and 31 August 2014. The relevant preoperative patient characteristics and clinical data are described in Table 1. The pre-operative aortic valve characteristics are detailed in Table 2.
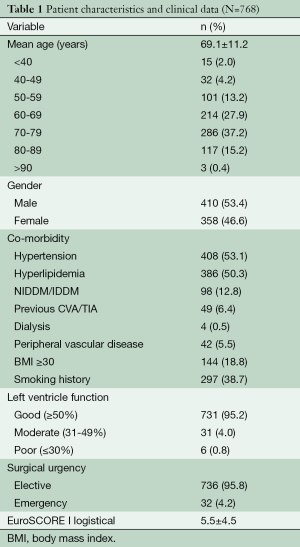
Full table
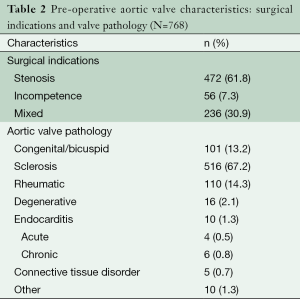
Full table
Surgical technique and in-hospital treatment pathway
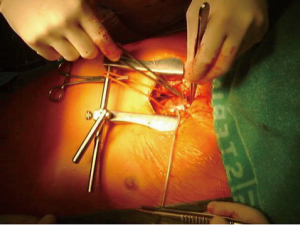
Our surgical technique for MI-AVS has been extensively described (3,13-16). We utilize a 4 to 8 cm midline skin incision starting at the manubrium-sternal joint and perform a partial upper JS-AVS with an oscillating saw down to either the 3rd or 4th right intercostal space depending on the patient body habitus (Figure 1).
We prefer direct antegrade ascending aortic cannulation and percutaneous femoral- and internal jugular venous cannulation via Seldinger technique (Figure 2). Combinations of femoral artery and vein cannulation through a 3 to 4 cm oblique incision in the groin may be used in selected patients with short aortas or impaired working space.

We use cold crystalloid cardioplegia in addition to mild systemic cooling (32 degrees) for myocardial protection. We induce cardioplegic arrest via the aortic root and maintain arrest by intermittent direct ostial cardioplegia delivery. Left ventricular distension is prevented by intermittent antegrade aortic root venting in cases of severe aortic valve incompetence.
Incision and closure of the aorta, valve excision and prosthetic implantation are all performed using standard instrumentation. Our de-airing strategy includes continuous CO2 flooding of the operative field, antegrade aortic root vent and transesophageal echocardiography (TEE) confirmation of de-airing efficiency in all cases.
Cardio-respiratory support, sedation and analgesia are administered as indicated in intensive care. Post-operative chest tubes are routinely removed 48 hours post-operatively and all patients receive structured in-hospital- and post-discharge rehabilitation.
Anti-coagulated therapy with fenprocoumon (3M Health Care Ltd) is initiated and stabilized in-hospital and continued for three months, with conversion to acetyl salicylic acid in the absence of persistent post-operative AF or mechanical valve implantation.
Follow-up
All patients attend an outpatient clinic 6-8 weeks post-operatively. In-hospital and 30-day outcomes were assessed by the incidence of adverse events.
Data analysis
All in-hospital data are collected prospectively. However, this study design was retrospective as the post-discharge data was collected retrospectively. Data are expressed as the mean ± standard deviation. Analysis was performed with SPSS Statistics 20.0 (IBM, USA). The authors had full access to the data and take responsibility for its integrity. All authors have read and agree to the manuscript as written.
Results
Intra-operative outcome
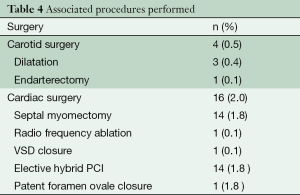
A total of 768 patients underwent primary isolated JS-AVS. Aortic valve replacement and repair were performed in 758 (98.7%) and 10 (1.3%) patients respectively. The technical characteristics, cardiopulmonary bypass- and cross-clamp times are outlined in Table 3. Associated procedures performed are described in Table 4. There were no early revisions for implantation related valve dysfunction.
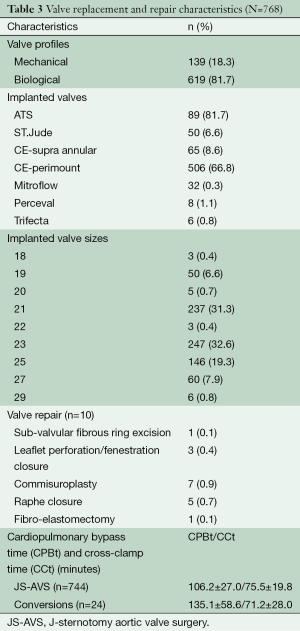
Full table
Full table
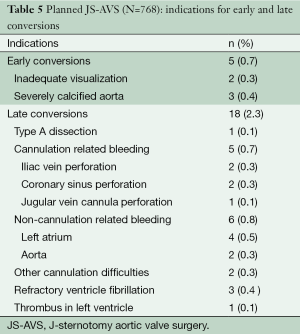
Early conversions occurred in five patients (0.7%) because of inadequate visualization or severely calcified aorta. Late intra-operative conversion occurred in 18 patients (2.3%) due to complications. The indications for early and late conversions are outlined in Table 5.
Full table
Post-operative course and outcome
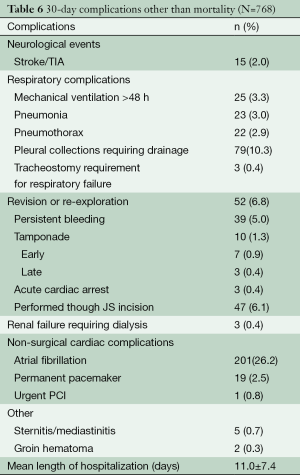
Total in-hospital mortality was 1.6% (n=12). Non-cardiac causes accounted for 0.7% (n=5) of in-hospital deaths, which included sepsis related multi-organ failure (n=3), fatal intra-pulmonary hemorrhage (n=1) and respiratory failure (n=1). Mechanical ventilation longer than 48 hours was required in 25 patients (3.3%) and three patients (0.4%) required respiratory support longer than seven days. The mean length of hospital stay was 11.0±7.5 days.
Overall 30-day mortality was 2.0% (n=15), which included three discharged patients who died of sudden cardiac arrest on post-operative days 15, 24 and 28 respectively. In-hospital complications and morbidities are outlined in Table 6.
Full table
Discussion
The excellent outcomes of current conventional surgical techniques for valvular disease set high standards for the implementation and development of new approaches and strategies, especially in view of an aging population with increased co-morbidities, operative risks and quality of life expectations (2).
Various centers now perform MI-AVS and reports that compare the outcomes of the different techniques are emerging. Minimally invasive techniques currently under investigation include right anterior thoracotomy (4,5,16), median mini-sternotomy with its variations (T-, J-, L-, reversed C-, S- and inverted V-shape) (3,6,8,11), off-pump implantation techniques through left anterior thoracotomy (17-23) and percutaneous aortic valve replacements (24,25).
We initiated our minimally invasive aortic valve program in October 1997 and established the partial upper JS-AVS approach as our preferred technique irrespective of body habitus, anatomical variation or risk profile. It offers circumferential access to the aorta and right atrium, even in obese patients. Indeed, 144 patients (18.8%) presented with body mass index (BMI) >30 and only five patients (0.7%) developed wound infection or sternal complications.
Early risk aversion conversion occurred in five patients (0.7%), whereas 18 patients (2.3%) required conversion due to an adverse intra-operative event. We consider the relative ease of conversion to full sternotomy an important advantage compared to other approaches.
Neurological events occurred in 15 patients (2.0%), with complete clinical recovery within 72 hours occurring in five patients (0.7%). This may be related to air embolism rather than organic micro-emboli. De-airing of the left ventricle is challenging and we strongly advocate continuous flooding of the operative field with CO2, antegrade aortic root venting and meticulous air surveillance by TEE.
Revisions (n=52, 6.8%) can be performed using the same incision, which we were able to perform in 90.4% (n=47 of 52) of our re-explorations. We performed no early valve implantation related revisions and have shown that the risk of patient-prosthesis mismatch is low (26).
Post-operative pneumothoraces and pleural collections occurred in 23 (3.0%) and 79 (10.3%) patients respectively despite meticulous efforts to maintain pleural integrity. Mechanical ventilation longer than 48 hours was required in 25 patients (3.3%) and three patients (0.4%) required respiratory support longer than seven days.
New onset atrial fibrillation (AF) occurred in 201 patients (26.2%). We avoid manipulation of the right atrial appendage and superior vena cava as a general operative principle. Age is a risk factor (27) and 406 patients (53%) were older than 70 years. Cardioplegia type does not appear to influence the prevalence (28,29).
We initiate and stabilize anticoagulation- and rehabilitation regimens in-hospital, which accounts for our length of hospitalization (11.0±7.4 days). The in-hospital and 30-day mortality in our series were 1.6% and 2.0% respectively.
Conclusions
Any new techniques require experience and repetition before optimal results are achieved. We believe that JS-AVS is an acceptable alternative in MI-AVS, has many technical advantages and good clinical outcomes.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Rosengart TK, Feldman T, Borger MA, et al. Percutaneous and minimally invasive valve procedures: a scientific statement from the American Heart Association Council on Cardiovascular Surgery and Anesthesia, Council on Clinical Cardiology, Functional Genomics and Translational Biology Interdisciplinary Working Group, and Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation 2008;117:1750-67. [PubMed]
- Phan K, Xie A, Di Eusanio M, et al. A meta-analysis of minimally invasive versus conventional sternotomy for aortic valve replacement. Ann Thorac Surg 2014;98:1499-511. [PubMed]
- Svensson LG. Minimal-access “J” or “j” sternotomy for valvular, aortic and coronary operations or re-operations. Ann Thorac Surg 1997;64:1501-3. [PubMed]
- Miceli A, Murzi M, Gilmanov D, et al. Minimally invasive aortic valve replacement using right minithoracotomy is associated with better outcomes than ministernotomy. J Thorac Cardiovasc Surg 2014;148:133-7. [PubMed]
- Glauber M, Miceli A, Bevilacqua S, et al. Minimally invasive aortic valve replacement via right anterior minithoracotomy: early outcomes and midterm follow-up. J Thorac Cardiovasc Surg 2011;142:1577-9. [PubMed]
- Karimov JH, Santarelli F, Murzi M, et al. A technique of an upper V-type ministernotomy in the second intercostal space. Interact Cardiovasc Thorac Surg 2009;9:1021-2. [PubMed]
- Schmitto JD, Mokashi SA, Cohn LH. Minimally-invasive valve surgery. J Am Coll Cardiol 2010;56:455-62. [PubMed]
- Tabata M, Umakanthan R, Cohn LH, et al. Early and late outcomes of 1000 minimally invasive aortic valve operations. Eur J Cardiothorac Surg 2008;33:537-41. [PubMed]
- Cosgrove DM III, Sabik JF. Minimally invasive approach for aortic valve operations. Ann Thorac Surg 1996;62:596-7. [PubMed]
- Bakir I, Casselman FP, Wellens F, et al. Minimally invasive versus standard approach aortic valve replacement: a study in 506 patients. Ann Thorac Surg 2006;81:1599-604. [PubMed]
- Bakir I, Casselman F, De Geest R, et al. Minimally invasive aortic root replacement: a bridge too far? J Cardiovasc Surg (Torino) 2007;48:85-91. [PubMed]
- Bakir I, Casselman FP, De Geest R, et al. Should minimally invasive aortic valve replacement be restricted to primary interventions? Thorac Cardiovasc Surg 2007;55:304-9. [PubMed]
- von Segesser LK, Westaby S, Pomar J, et al. Less invasive aortic valve surgery: rationale and technique. Eur J Cardiothorac Surg 1999;15:781-5. [PubMed]
- Cohn LH, Adams DH, Couper GS, et al. Minimally invasive cardiac valve surgery improves patient satisfaction while reducing costs of cardiac valve replacement and repair. Ann Surg 1997;226:421-6; discussion 427-8. [PubMed]
- Doll N, Borger MA, Hain J, et al. Minimal access aortic valve replacement: effects on morbidity and resource utilization. Ann Thorac Surg 2002;74:S1318-22. [PubMed]
- Ruttmann E, Gilhofer TS, Ulmer H, et al. Propensity score-matched analysis of aortic valve replacement by mini-thoracotomy. J Heart Valve Dis 2010;19:606-14. [PubMed]
- Walther T, Dewey T, Wimmer-Greinecker G, et al. Transapical approach for sutureless stent-fixed aortic valve implantation: experimental results. Eur J Cardiothorac Surg 2006;29:703-8. [PubMed]
- Huber CH, Cohn LH, von Segesser LK. Direct-access valve replacement a novel approach for off-pump valve implantation using valved stents. J Am Coll Cardiol 2005;46:366-70. [PubMed]
- Huber CH, von Segesser LK. Direct access valve replacement (DAVR) - are we entering a new era in cardiac surgery? Eur J Cardiothorac Surg 2006;29:380-5. [PubMed]
- Walther T, Falk V, Borger MA, et al. Minimally invasive transapical beating heart aortic valve implantation--proof of concept. Eur J Cardiothorac Surg 2007;31:9-15. [PubMed]
- Lichtenstein SV, Cheung A, Ye J, et al. Transapical transcatheter aortic valve implantation in humans: initial clinical experience. Circulation 2006;114:591-6. [PubMed]
- Gammie JS, Brown JW, Brown JM, et al. Aortic valve bypass for the high-risk patient with aortic stenosis. Ann Thorac Surg 2006;81:1605-10. [PubMed]
- Vassiliades TA Jr. Off-pump apicoaortic conduit insertion for high-risk patients with aortic stenosis. Eur J Cardiothorac Surg 2003;23:156-8. [PubMed]
- Webb JG, Chandavimol M, Thompson CR, et al. Percutaneous aortic valve implantation retrograde from the femoral artery. Circulation 2006;113:842-50. [PubMed]
- Miller DC, Blackstone EH, Mack MJ, et al. Transcatheter (TAVR) versus surgical (AVR) aortic valve replacement: occurrence, hazard, risk factors, and consequences of neurologic events in the PARTNER trial. J Thorac Cardiovasc Surg 2012;143:832-843.e13.
- Hogue CW Jr, Hyder ML. Atrial fibrillation after cardiac operation: risks, mechanisms, and treatment. Ann Thorac Surg 2000;69:300-6. [PubMed]
- Mathew JP, Parks R, Savino JS, et al. Atrial fibrillation following coronary artery bypass graft surgery: predictors, outcomes, and resource utilization. MultiCenter Study of Perioperative Ischemia Research Group. JAMA 1996;276:300-6. [PubMed]
- Asher CR, DiMengo JM, Arheart KL, et al. Atrial fibrillation early postoperatively following minimally invasive cardiac valvular surgery. Am J Cardiol 1999;84:744-7, A9.
- Bakir I, Casselman FP, Onan B, et al. Does a minimally invasive approach increase the incidence of patient-prosthesis mismatch in aortic valve replacement? J Heart Valve Dis 2014;23:161-7. [PubMed]