Evolving strategies in the treatment of acute myocardial infarction-induced cardiogenic shock
Introduction
Acute cardiogenic shock (CS) is a state of cardiac failure resulting in end–organ hypoperfusion. The diagnosis of acute CS can include hemodynamic parameters, laboratory data, as well as clinical manifestations of cardiac failure. This consists of: (I) systolic blood pressure <90 mmHg and/or mean arterial pressure <30 mmHg; (II) cardiac index of <1.8 L/min/m2 or <2.2 L/min/m2 while using inotropic support; (III) decreased urine output; and (IV) altered mental status (1). Although the etiology of acute CS may be multifaceted, the reversible or irreversible causes must be elucidated in order to identify the ideal treatment strategy.
The most prevalent etiology of acute CS is myocardial infarction. There are approximately 40,000-50,000 cases of acute myocardial infarction cardiogenic shock (AMICS) per year in the United States (1). In the majority of patients (80%), shock is the result of left-sided pump failure. It is important to exclude other contributory factors, such as valvular insufficiency, septal or free wall rupture (2).
AMICS and revascularization
The most prevalent treatment strategy for AMICS is early revascularization, as evidenced by the SHOCK Trial (should we emergently revascularize Occluded Coronaries for CS) (3). The SHOCK trial revealed significant improvement in 6 months (3) and 1 year (4) survival in the early revascularization group versus the group that received medical treatment. However, the primary end-point, 30-day mortality, was not statistically significantly different between the two groups (survival 56.0% vs. 46.7%, P=0.11) (3). More recent studies of AMICS have revealed a temporal improvement in survival with early revascularization, but overall index hospitalization mortality remains 50% (1).
Unfortunately, the current treatment paradigms are unable to discern patients who will or will not benefit from revascularization. The emphasis is to reperfuse all despite a relative ongoing high mortality rate. In an effort to reduce the mortality following AMICS, the emphasis has been placed on early revascularization to salvage as much myocardium as possible (5). Current guidelines recommend a door-to balloon time of less than 90 minutes for patients requiring primary percutaneous coronary intervention (PCI) (6). Door-to balloon time has become a key performance indicator and is the focus of regional and national quality-improvement initiatives (7). However, despite shorter door-to-balloon times, these incremental improvements have not translated into a lower mortality (8).
The groundwork for our program
Our current treatment strategy evolved from the premise that AMICS mortality remains unacceptably high, and that the majority of mortality is attributable to left sided pump failure (9-11). Coincident to the development of this premise was the evolution in the technology of mechanical circulatory support (MCS). It did not seem reasonable that there was a substantial population of patients dying from acute left ventricular failure despite significant improvements in the technology available to reliably restore normal hemodynamics for prolonged periods. Thus, our focus shifted away from the heart to first and foremost saving the “organism”.
In the development of our protocols using MCS to treat refractory AMICS, we applied concepts learned from trauma surgery. The “Golden Hour”, though not scientifically validated, is widely adopted to limit the systemic inflammatory response and subsequent multi-organ dysfunction, sepsis and death (12). Our application of this tenet to MCS during refractory AMICS re-emphasizes the importance of maintaining adequate hemodynamics and tissue perfusion for the organism, as the function provided by the heart can be replaced. Previous studies have demonstrated that the development of multi-organ dysfunction prior to MCS support results in an increased mortality (13). Within our institution, we have identified decreased urine output, elevated transaminases, elevated total bilirubin, fever, elevated WBC and CRP as predictors of increased mortality at the time of implant (Teeters J.C., unpublished data).
In addition to using MCS to support the hemodynamics and maintain adequate tissue perfusion, recent data has suggested that unloading the heart during AMICS may improve myocardial recovery. The results of Kapur et al. make a compelling case to pursue newer treatment paradigms in limiting reperfusion injury and actually improving myocardial salvage (14). MCS offers the advantage of maintaining normal hemodynamics while decreasing myocardial metabolic demand during a time of targeted therapy, to limit reperfusion injury and increase myocardial recovery. Thus, it reinforces the concept of saving both the organism and the organ.
Treatment strategy
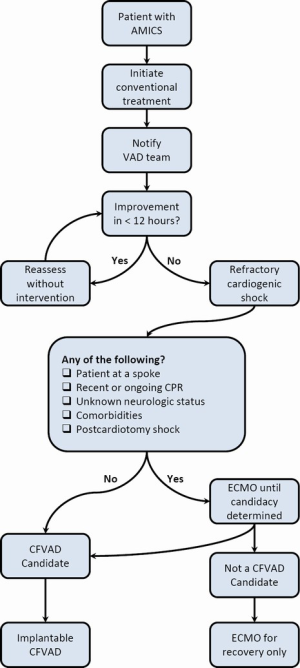
The primary goal of using MCS support during AMICS is the early identification of patients who would not survive after conventional therapy. The challenge has always been applying the therapy to those who truly require it, at the time point at which they can survive an additional insult from the implant procedure. Historically, this was more difficult, given the significant risks and limited durability of the technology available (15). Following the diagnosis of AMICS, at least 50% of the deaths occur within the first 48 hours of being diagnosed with cardiogenic shock (2,16,17). All patients that have the diagnosis of AMICS following conventional therapy are urgently assessed by the MCS team and are continually reassessed over the ensuing 12 hours (Figure 1). Medical therapy is optimized in all patients and continual hemodynamic monitoring, laboratory data, and clinical manifestations of shock are evaluated hourly. In those patients who remain in clinically refractory cardiogenic shock and fail to respond to conventional measures as evidenced by failure to wean inotropes, escalating inotropes or marginal hemodynamics, the decision is to proceed with implantable continuous flow MCS support within this 12 hour time-frame. In those patients who respond to conventional therapy with a de-escalation of support and stable hemodynamics, the MCS team continues to evaluate on an ongoing basis until fully stabilized. Veno-arterial extracorporeal membrane oxygenation (VA-ECMO) is administered in patients who have suffered cardiorespiratory arrest requiring cardiopulmonary resuscitation (CPR), have an unknown neurologic status, and/or have received lytic therapy or anticoagulant therapy that places them at high risk for substantial surgical bleeding. VA-ECMO is also utilized in patients who are not deemed candidates for implantable continuous-flow left ventricular assist device (CF LVAD) therapy due to underlying co-morbidities (cirrhosis, chronic obstructive pulmonary disease, significant peripheral vascular disease, cerebrovascular accident), lack of social support, substance abuse issues, or patient preference as a bridge to potential cardiac recovery. Treatment goals and end-points are clearly established with the admitting service and family prior to establishing support.
Initiation of VA-ECMO
As demonstrated by Figure 1, patients in refractory AMICS, who are not current candidates for CF LVAD therapy, undergo stabilization with peripheral VA ECMO with a centrifugal (CF) pump (CentriMag, RotoFlow) and Quadrox oxygenator system. The VA-ECMO system utilizes a heparin bonded circuit, and is simplified without pre- or post-oxygenator ports or pressure monitors.
Outflow cannulation is achieved by directly cannulating the subclavian artery with a 19 or 21 Fr outflow cannula through a small cut-down incision. Preferentially using the subclavian artery over the femoral artery has resulted in less limb ischemia, and avoids the problem of differential perfusion cyanosis. The outflow cannula is tunneled from outside of the incision and directly placed into the subclavian artery using the Seldinger technique, and its position is verified using trans-esophageal echocardiography (TEE). The cannula is then secured using two 4-0 polypropylene purse-string sutures. In our experience, an end-to-side T-graft sewn onto the subclavian artery tends to have more bleeding complications due to pressurization of the graft and anastomosis. In addition, a T-graft configuration can occasionally result in hyperperfusion of the right upper extremity and subsequent compartment syndrome. Inflow cannulation is achieved using a percutaneously placed femoral venous inflow (21-25 Fr) which can be subsequently adjusted at the bedside to optimize flow.
Anticoagulation for initial VA ECMO cannulation includes an activated clotting time (ACT) of >300 seconds unless otherwise contraindicated. Once VA-ECMO flows have been established, heparin is fully reversed using protamine. Re-initiation of heparin begins after 24 hours to achieve a target ACT of 160-180 seconds.
VA-ECMO and left ventricular unloading
Following VA-ECMO initiation arterial waveform morphology, TEE and Swan-Ganz catheters provide assessment for left ventricular unloading. A pulmonary capillary wedge pressure greater than 20 mmHg, absent systemic arterial waveform pulsatility, intermittent or absent opening of the aortic valve, left ventricular dilation, or ECHO smoke are all indications that the left ventricle is inadequately unloaded. It is imperative to urgently unload the left ventricle to prevent the sequelae of cardiac thrombosis, pulmonary venous hypertension and pulmonary micro-vascular injury.
The options we use to unload the left ventricle during VA-ECMO are either a transaortic Impella 2.5 (Abiomed; Danvers, MA, USA) (18), or direct left ventricular vent. We have previously shown that the Impella 2.5 will significantly decrease the left ventricular end diastolic diameter, and pulmonary capillary wedge pressure in patients requiring VA-ECMO (19). It is additionally attractive as it does not require an incision but has limitations of secure positioning and hemolysis.
This VA-ECMO strategy provides flows of 4-6 L/min without significant hemolysis (average lactate dehydrogenase 300-500 units). Treatment goals and end-points are clearly established with the admitting service and family prior to establishing support. The VA-ECMO system is utilized for initial stabilization for 3-10 days to determine suitability for further therapy or recovery.
Continuous-flow left ventricular assist device (CF LVAD)
At our institution, we currently and for the past six years have used the HeartMate II (Thoratec; Pleasanton, CA, USA) CF LVAD in conjunction with a CentriMag RVAD if required for temporary RV support. (Thoratec; Pleasanton, CA, USA) (20). The left ventricular apex should be cored in the standard fashion, and the inflow cannula/cuff secured using large bites of pledgeted 2-0 braided polyester sutures. Care is taken to tie each suture firmly, but without excess tension to prevent tearing through the necrotic myocardium. Diligent examination of the left ventricular cavity should be performed to rule out thrombus. The continuous direct unloading of the left ventricle with the newer generation of implantable CF LVADs has been advantageous in reducing bleeding complications from the LV apical coring site.
In refractory AMICS, pre-operative echocardiography may well reveal a “normally” functioning right ventricle (RV). However, in our experience, subsequent RV failure is not uncommon. The majority of patients with refractory AMICS have left anterior descending coronary artery disease (21) therefore involving the septal distribution. As previously described, a significant part of RV function is derived from the LV and the septum (15,22-25), and thus the RV is inherently dysfunctional due to loss of septal contribution. The echocardiography may underestimate the degree of RV dysfunction due to retained free wall contractility and low stroke volumes prior to initiating CF LVAD support. In addition, preoperative pulmonary edema and post-operative fluid shifts and, transfusions place the patient with refractory AMICS at increased risk for requiring temporary RVAD support. In selected patients, after implant of CF-LVAD, a CentriMag RVAD is implanted in a configuration that allows for remote decannulation (20). This allows for earlier sternal stabilization and mobilization of the patient (26). Use of this approach has led to explantation of 91.8% of RVADs, an 88% hospital survival, and 77% one year survival (20).
Perspective and conclusions
Despite the success from our group and others using MCS following refractory AMICS, there is a lack of adequately powered randomized trials and accepted protocols. The use of MCS in AMICS is haphazard at best. Only recently was MCS considered in the treatment paradigm of AMICS in the AHA/ACC guidelines (27). Despite the origins of MCS from the support of patients in acute CS, there have been no significant trials in the modern era to address this population. The only FDA-approved devices for the use in CS are of limited durability and not the newer second and third generation implantable CF LVADs (28). Previously, the bridge to determinacy indication offered an entry point for patients with AMICS into the pathway for the newer generation CF LVADs. However, there have been recent determinations by Medicare not to recognize bridge to determinacy (28). This lack of interest in directly studying the AMICS population in clinical trials has remained somewhat confounding, considering that >50% of patients currently implanted with the newer generation CF LVADs are INTERMACS levels 1/2 (16.6% and 36.7% respectively) and by definition are in critical CS or require continuous inotropes (29).
We have demonstrated improved success in using MCS in patients with refractory CS following myocardial infarction. With the MCS field continually evolving, our hope is that other groups will develop protocols to treat this difficult group of patients with the goal to improve the 50% survival which has remained relatively unchanged within the past two decades.
Acknowledgements
Disclosure: HTM is a consultant for Thoratec Corporation (Pleasanton, CA, USA), and SynCardia Systems, Inc. (Tucson, AZ, USA). The authors declare no conflict of interest.
References
- Reynolds HR, Hochman JS. Cardiogenic shock: current concepts and improving outcomes. Circulation 2008;117:686-97. [PubMed]
- Hochman JS, Buller CE, Sleeper LA, et al. Cardiogenic shock complicating acute myocardial infarction--etiologies, management and outcome: a report from the SHOCK Trial Registry. SHould we emergently revascularize Occluded Coronaries for cardiogenic shocK? J Am Coll Cardiol 2000;36:1063-70. [PubMed]
- Hochman JS, Sleeper LA, Webb JG, et al. Early revascularization in acute myocardial infarction complicated by cardiogenic shock. SHOCK Investigators. Should We Emergently Revascularize Occluded Coronaries for Cardiogenic Shock. N Engl J Med 1999;341:625-34. [PubMed]
- Hochman JS, Sleeper LA, White HD, et al. One-year survival following early revascularization for cardiogenic shock. JAMA 2001;285:190-2. [PubMed]
- Brodie BR, Stuckey TD, Muncy DB, et al. Importance of time-to-reperfusion in patients with acute myocardial infarction with and without cardiogenic shock treated with primary percutaneous coronary intervention. Am Heart J 2003;145:708-15. [PubMed]
- Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction--executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). Circulation 2004;110:588-636. [PubMed]
- Bradley EH, Herrin J, Wang Y, et al. Strategies for reducing the door-to-balloon time in acute myocardial infarction. N Engl J Med 2006;355:2308-20. [PubMed]
- Menees DS, Peterson ED, Wang Y, et al. Door-to-balloon time and mortality among patients undergoing primary PCI. N Engl J Med 2013;369:901-9. [PubMed]
- Risk stratification and survival after myocardial infarction. N Engl J Med 1983;309:331-6. [PubMed]
- Rouleau JL, Talajic M, Sussex B, et al. Myocardial infarction patients in the 1990s--their risk factors, stratification and survival in Canada: the Canadian Assessment of Myocardial Infarction (CAMI) Study. J Am Coll Cardiol 1996;27:1119-27. [PubMed]
- La Rovere MT, Bigger JT Jr, Marcus FI, et al. Baroreflex sensitivity and heart-rate variability in prediction of total cardiac mortality after myocardial infarction. ATRAMI (Autonomic Tone and Reflexes After Myocardial Infarction) Investigators. Lancet 1998;351:478-84. [PubMed]
- Crowley RA. The resuscitation and stabilization of major multiple trauma patients in a trauma center environment. Clin Med 1976;83:16-22.
- Holman WL, Kormos RL, Naftel DC, et al. Predictors of death and transplant in patients with a mechanical circulatory support device: a multi-institutional study. J Heart Lung Transplant 2009;28:44-50. [PubMed]
- Kapur NK, Paruchuri V, Urbano-Morales JA, et al. Mechanically unloading the left ventricle before coronary reperfusion reduces left ventricular wall stress and myocardial infarct size. Circulation 2013;128:328-36. [PubMed]
- Hoffman D, Sisto D, Frater RW, et al. Left-to-right ventricular interaction with a noncontracting right ventricle. J Thorac Cardiovasc Surg 1994;107:1496-502. [PubMed]
- Webb JG, Sanborn TA, Sleeper LA, et al. Percutaneous coronary intervention for cardiogenic shock in the SHOCK Trial Registry. Am Heart J 2001;141:964-70. [PubMed]
- Jeger RV, Harkness SM, Ramanathan K, et al. Emergency revascularization in patients with cardiogenic shock on admission: a report from the SHOCK trial and registry. Eur Heart J 2006;27:664-70. [PubMed]
- Impella 2.5. Abiomed. Available online: http://www.abiomed.com/products/impella-2-5/. Accessed April 28, 2014.
- Cheng A, Swartz MF, Massey HT. Impella to unload the left ventricle during peripheral extracorporeal membrane oxygenation. ASAIO J 2013;59:533-6. [PubMed]
- Lazar JF, Swartz MF, Schiralli MP, et al. Survival after left ventricular assist device with and without temporary right ventricular support. Ann Thorac Surg 2013;96:2155-9. [PubMed]
- Wong SC, Sanborn T, Sleeper LA, et al. Angiographic findings and clinical correlates in patients with cardiogenic shock complicating acute myocardial infarction: a report from the SHOCK Trial Registry. SHould we emergently revascularize Occluded Coronaries for cardiogenic shocK? J Am Coll Cardiol 2000;36:1077-83. [PubMed]
- Santamore WP, Dell'Italia LJ. Ventricular interdependence: significant left ventricular contributions to right ventricular systolic function. Prog Cardiovasc Dis 1998;40:289-308. [PubMed]
- Klima UP, Lee MY, Guerrero JL, et al. Determinants of maximal right ventricular function: role of septal shift. J Thorac Cardiovasc Surg 2002;123:72-80. [PubMed]
- Damiano RJ Jr, La Follette P Jr, Cox JL, et al. Significant left ventricular contribution to right ventricular systolic function. Am J Physiol 1991;261:H1514-24. [PubMed]
- Starr I, Jeffers WA, Meade RH. The absence of conspicuous increments of venous pressure after severe damage to the right ventricle of the dog, with a discussion of the relation between clinical congestive failure and heart disease. Am Heart J 1943;26:291-301.
- Lazar JF, Schiralli M, Pisula B, et al. Does Treating Acute Cardiogenic Shock with Biventricular Assist Devices Improve Survival: A Single In stitution Review, ASAIO Cardiac Abstracts. ASAIO J 2012;58;20-45. Supplement 17.
- O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2013;127:e362-425. [PubMed]
- Centers for Medicare & Medicaid Services. National Coverage Determination (NCD) for Artificial Hearts and Related Devices, Centers for Medicare & Medicaid Services. Available online: http://www.cms.gov/medicare-coverage-database/details/ncd-details.aspx?NCDId=246&ncdver=5&NCAId=211&ver=20&NcaName=Artificial+Hearts&bc=ACAAAAAAIAAA&. Accessed April 26, 2014.
- Kirklin JK, Naftel DC, Kormos RL, et al. Fifth INTERMACS annual report: risk factor analysis from more than 6,000 mechanical circulatory support patients. J Heart Lung Transplant 2013;32:141-56. [PubMed]





