Clinical outcomes of hybrid repair for thoracoabdominal aortic aneurysms
Abstract
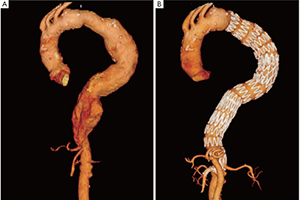
Background: Thoracoabdominal aortic aneurysm (TAAA) hybrid repair consists of aortic visceral branch rerouting followed by TAAA endograft exclusion. This technique has been shown to represent a technically feasible strategy in selected patients.
Methods: We analyzed 52 high-risk patients who underwent hybrid TAAA repair between 2001 and 2012 in our Center with a variety of visceral rerouting configurations and of commercially available thoracic endografts. Thirty-seven simultaneous (71.2%) and 15 staged procedures (21.8%) were performed with a four-vessel revascularization in 18 cases (34.6%), a three-vessel revascularization in 11 cases (21.2%) and a two-vessel revascularization in 23 cases (44.2%).
Results: No intraoperative deaths were observed. We recorded a perioperative mortality rate of 13.5% (n=7), including deaths from multiorgan failure (n=2), myocardial infarction (n=2), coagulopathy (n=1), pancreatitis (n=1) and bowel infarction (n=1). Perioperative morbidity rate was 28.8% (n=15), including 2 cases of transient paraparesis and 1 case of permanent paraplegia. Renal failure (n=5), pancreatitis (n=3), respiratory failure (n=3) and dysphagia (n=1) were also observed. At median follow-up of 23.9 months procedure-related mortality rate was 9.6%: two patients died from visceral graft occlusion and three from aortic rupture. There were three endoleaks and one endograft migration, none of which resulted in death. Five patients (9.6%) died as a consequence of unrelated events.
Conclusions: Typical complications of conventional TAAA open surgery have not been eliminated by hybrid repair, and significant mortality and morbidity rates have been recorded. Fate of visceral bypasses and incidence of endoleak and other endograft-related complications needs to be carefully assessed. Hybrid TAAA repair should currently be limited to high-risk surgical patients with unfit anatomy for endovascular repair.
Cover