Ministernotomy or minithoracotomy for minimally invasive aortic valve replacement: a Bayesian network meta-analysis
Introduction
Minimally invasive aortic valve surgery (MIAVR) has been increasingly accepted in the surgical community as a potential alternative to conventional sternotomy, with advantages of reduced trauma, improved cosmesis and reduced hospitalization (1,2). Ministernotomy (MS) is the most common approach to MIAVR and involves a small incision of the sternum, thus allowing access to the cardiac structures (Figure 1). However, more recent studies have described the minithoracotomy (MT) approach, which involves an incision between the ribs of the right chest to allow access to the heart (3-5). While several meta-analyses (6) and randomized trials (7-10) to date have demonstrated similar safety and efficacy between MIAVR and conventional aortic valve replacement (CAVR), there are few studies available which have directly compared MS and MT approaches. As such, the decision for selecting the MS or MT approach has largely been based on the surgeon’s preference.
Network meta-analysis is a Bayesian statistical approach which allows comparison of two treatments or interventions by pooling together a full network of direct head-to-head and indirect evidence to produce a single, integrated effect estimate (11-13). The lack of robust clinical evidence directly comparing MS and MT necessitates a contemporary appraisal and thus, a network meta-analysis was performed to evaluate the current evidence base.
Materials and methods
Literature search strategy
Electronic searches were performed using Ovid Medline, PubMed, Cochrane Central Register of Controlled Trials (CCTR), Cochrane Database of Systematic Reviews (CDSR), ACP Journal Club, and Database of Abstracts of Review of Effectiveness (DARE) from their date of inception to June 2014. To achieve the maximum sensitivity of the search strategy and identify all studies, we combined the terms “minimally invasive” OR “ministernotomy” OR “hemisternotomy” OR “partial sternotomy” OR “minithoracotomy” OR “partial thoracotomy” AND “aortic valve” AND “surgery” as either key words or MeSH terms. The reference lists of all retrieved articles were reviewed for further identification of potentially relevant studies. All identified articles were systematically assessed using the inclusion and exclusion criteria.
Selection criteria
Eligible randomized controlled trials (RCTs) and propensity-score matched trials for the present systematic review and meta-analysis included those in which patient cohorts underwent minimally invasive aortic valve replacement via MS or MT versus aortic valve replacement by conventional sternotomy (CS). Studies that did not have randomized or propensity-matched cohorts were excluded. When institutions published duplicate studies with accumulating numbers of patients or increased lengths of follow-up, only the most complete reports were included for quantitative assessment at each time interval. All publications were limited to those involving human subjects. Abstracts, case reports, conference presentations, editorials, reviews and expert opinions were excluded.
Data extraction and appraisal
All data were extracted from article texts, tables and figures. Two investigators independently reviewed each retrieved article (K.P. and A.X.). Discrepancies between the two reviewers were resolved by discussion and consensus. The final results were reviewed by the senior investigators (M.D.E., T.D.Y.).
Traditional meta-analysis
For traditional pair-wise meta-analysis, the relative risk (RR) was used as a summary statistic. In the present study, both fixed- and random-effect models were tested. χ2 tests were used to study heterogeneity between trials. I2 statistic was used to estimate the percentage of total variation across studies, owing to heterogeneity rather than chance, with values greater than 50% considered as substantial heterogeneity. If there was substantial heterogeneity, the possible clinical and methodological reasons for this were explored qualitatively. In the present meta-analysis the results using the random-effects model were presented to take into account the possible clinical diversity and methodological variation between studies. Weighted Pearson’s coefficient (rs) was used to calculate correlation coefficients for meta-regression analysis of outcomes based on midpoint of study periods. All levels of significance (α) were two-sided.
Bayesian network meta-analysis
A Bayesian network meta-analysis was carried out to make indirect comparisons among treatments (MS vs. MT vs. CS) when direct comparisons were scarce. Estimates of relative effects and all model parameters were obtained via a random-effects network within a Bayesian framework using Markov Chain Monte Carlo simulation from the posterior distributions. Four parallel Markov Chain Monte Carlo simulations were run for a period of at least 50,000 interactions, until convergence was obtained. Inconsistency of evidence was assessed using node-splitting analysis when possible.
All analyses were conducted using R version 2.15.2 and GeMTC package version 0.4. If the difference between random effects variance and inconsistency variance was large (P<0.05), then significant heterogeneity was present.
Results
Quality of included studies
Our literature search identified 17 relevant studies, including seven randomized controlled trials (7,8,10,14-17) and ten propensity-score matched observational studies (4,18-26) (Table 1). A total of 6,516 patients were analysed, including 3,258 in the MIAVR group and 3,258 in the CAVR group. Seven studies included at least 100 patients in each arm (4,18-20,22,25,26), while ten studies included fewer than 100 patients in each arm (7,8,10,14-17,21,23,24). MS was directly compared with CS in 12 studies (7,8,10,15-19,21,22,24,26), while five studies (4,14,20,23,25) directly compared MT with CS. There were no randomized or propensity-matched studies that directly compared MS with MT approaches. Three studies reported mean or median follow-up greater than 12 months (4,18,22).
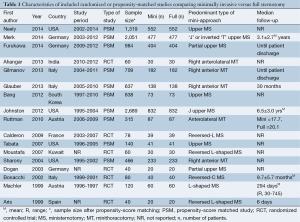
Full table
The cardiopulmonary bypass (CPB) duration was reported in all studies except one (10), while cross-clamp duration was reported in all studies. The total operation duration was reported in nine studies (7,8,10,14-16,18,19,23). Early mortality (30-day) was reported in all studies except one (14). Stroke outcomes were not reported in five studies (7,8,10,14,17), while reoperation for bleeding outcomes were not reported in three studies (14,17,18). Wound infection rates were reported in all studies except three (7,19,26). Other outcomes including transfusions, atrial fibrillation, pacemaker implantations, myocardial infarctions, tamponade, pneumonia, pleural effusions, respiratory and renal failures were reported in fewer than 10 studies, and these outcomes were considered to have insufficient data for Bayesian network meta-analysis in the present study.
Assessment of operational data
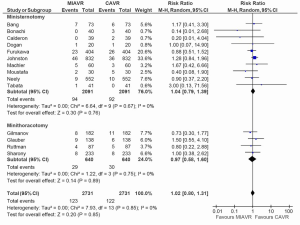
Across all included studies using traditional pairwise meta-analysis, there was no significant difference in CPB duration between MIAVR and CAVR cohorts (WMD, 4.00; 95% CI, –2.15-10.15; P=0.20; I2=94%). For the MS subgroup, this trend was maintained with no difference in CPB duration between cohorts (WMD, 0.47; 95% CI, –7.02-7.97; P=0.80; I2=94%). However, CPB duration was found to be significantly longer in the MT subgroup compared with matched CAVR patients (WMD, 9.99; 95% CI, 3.91-16.07; I2=55%; P=0.001) (Figure 2). Bayesian network meta-analysis did not show significant differences between MS and MT approaches (WMD, –9.59; 95% CI, –24.03-5.47; Table 2).

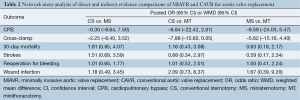
Full table
Pairwise meta-analysis demonstrated that MIAVR had significantly longer cross-clamp duration than CAVR (WMD, 4.01; 95% CI, 0.31-7.70; P=0.03; I2=93%) (Figure 3). Subgroup analysis showed that this difference was only significant in the MT group (WMD, 7.64; 95% CI, 2.86-12.42; P=0.002; I2=74%) and not the MS group. A similar trend was obtained via Bayesian analysis, where the difference between the MT and CAVR groups almost reached significance (WMD, –7.88; 95% CI, –15.60-0.05; Table 2).
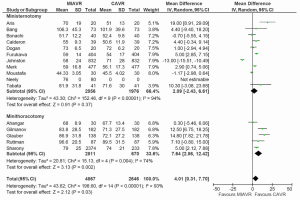
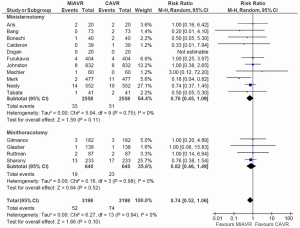
Assessment of mortality
There was no difference in 30-day mortality rates between MIAVR and CAVR across all included studies (RR, 0.74; 95% CI, 0.52-1.06; P=0.10; I2=0%). From subgroup analysis, there was also no difference between MS and CAVR (RR, 0.70; 95% CI, 0.45-1.09; P=0.11; I2=0%) or MT and CAVR (RR, 0.82; 95% CI, 0.46-1.49; P=0.52; I2=0%) (Figure 4). Similar results were obtained using network meta-analysis, with no difference between MS and MT detected (OR, 0.63; 95% CI, 0.18-2.17; Table 2).
Assessment of safety
From the studies included for analysis of stroke outcomes, no difference was detected between MIAVR and CAVR cohorts (RR, 0.81; 95% CI, 0.55-1.21; P=0.31; I2=0%) (Figure 5). Subgroup testing via pairwise analysis did not reveal differences between MS and CS (RR, 0.74; 95% CI, 0.47-1.17; P=0.20; I2=0%) or MT and CS (RR, 1.09; 95% CI, 0.48-2.51; P=0.83; I2=0%). Likewise for reoperations for bleeding, no difference was found between MIAVR and CAVR overall (RR, 1.02; 95% CI, 0.80-1.31; P=0.85; I2=0%) (Figure 6), nor was there any difference between MS and CS (RR, 1.04; 95% CI, 0.79-1.39; P=0.76) or MT and CS (RR, 0.97; 95% CI, 0.58-1.60; P=0.89). Wound infection rates were also found to be equivalent when comparing MS with CS (RR, 0.83; 95% CI, 0.39-1.76; P=0.62) and MT with CS (RR, 0.60; 95% CI, 0.25-1.43; P=0.25) (Figure 7).
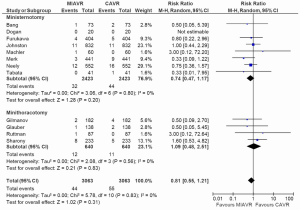
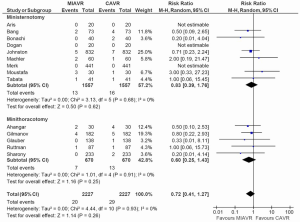
From network multiple-treatment meta-analysis, there was equivalent safety between MS and MT in terms of stroke (OR, 0.63; 95% CI, 0.18-2.17), reoperation for bleeding (OR, 1.00; 95% CI, 0.41-2.24), and wound infection rates (OR, 1.67; 95% CI, 0.39-9.20).
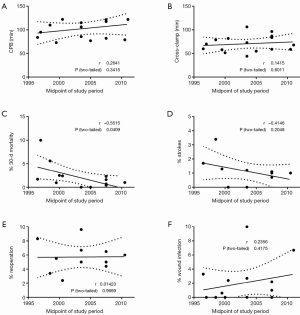
Meta-regression analysis
Random effects meta-regression analysis considering variables of interest one at a time showed that midpoint of study period only significantly negatively correlated with 30-day mortality rates (Pearson’s coefficient, r=–0.5515; P=0.0409; Figure 8). No significant correlation was found between midpoint of study period and CPB duration (P=0.3415), cross-clamp duration (P=0.6011), stroke (P=0.2048), reoperation for bleeding (P=0.9669) and wound infection rates (P=0.4175).
Discussion
There have been few studies to date that have discussed the results of MS versus MT for MIAVR directly. In the only direct comparative study, Miceli et al. (27) investigated 251 MT and 155 MS patients and concluded that MT was associated with lower postoperative atrial fibrillation and shorter hospitalization. In contrast, subgroup analysis of a recent meta-analysis (2) suggested that MS may be associated with superior mortality outcomes compared to MT patients. These studies are susceptible to the inherent biases of non-randomized, observational designs that make it difficult to conclusively compare the different surgical approaches. Furthermore, conventional direct meta-analysis fails to measure the relative efficacy of MS, MT and CS, as it only synthesizes studies with the same comparator group. Instead, a Bayesian network meta-analysis can be used to provide a valid statistical comparison between different interventions by combining the network of direct head-to-head and indirect comparative evidence (11,12). As such, both traditional frequentist and Bayesian chain meta-analysis of higher quality randomized and propensity score-matched studies were performed to assess the relative safety and efficacy of MS, MT and CS.
While MS had similar CPB and cross-clamp duration compared with CS, MT was associated with significantly longer CPB and cross-clamp durations. There are several reasons as to why partial thoracotomy may be associated with slightly longer operational outcomes. Firstly, compared to MS and CS, MT may provide a limited vision of the aortic valve due to greater distance from the thoracic access. This may reduce maneuverability and increase the difficulty of using long-shaft instruments. The increased complexity of the MT procedure compared to MS and CS approaches could also explain the longer bypass and cross-clamp durations observed. Furthermore, the MT approach has only been used extensively in recent years, with a greater number of centers now experienced with the MS approach, thus traversing the learning curve associated with minimally invasive surgical techniques. While the evidence indicates that MT operations may be longer, it is important to note that the absolute difference is approximately 10 and 5 minutes for CPB and cross-clamp respectively, which may not be clinically significant. The increasing use of sutureless implantation technique may facilitate these minimally invasive approaches in the future, and thus may reduce CPB and cross-clamp durations even further (28). However, whether sutureless AVR is associated with comparable short and long term results with conventional AVR remains to be investigated by prospective randomized studies.
Randomized and propensity-matched evidence to date suggests that MIAVR is an equally safe and efficacious alternative to median sternotomy for aortic valve replacement. No significant differences in 30-day mortality, stroke, reoperations for bleeding and wound infections were found for MIAVR overall. These results were also consistent with Bayesian network meta-analysis, suggesting that both MS and MT approaches are safe, efficacious and comparable. There have been some previous concerns that the standard MT approach requires retrograde arterial perfusion through the femoral artery, which has been associated with increased risk of stroke (29,30). However, this risk is not consistently reported across the literature, with other institutions reporting excellent stroke outcomes with femoral cannulation (31). Given the inconsistent data available on femoral versus central cannulation, it is likely that the optimal cannulation strategy should be individualized to the specific patient. Retrograde arterial flow can also lead to iliac artery dissections, another complication which may be associated with MT and can lead to increased mortality rates. Thus MS utilizing central aortic cannulation may also result in improved safety and mortality outcomes. In contrast to MS which involves a small sternal incision, MT avoids incision of the sternum and rib bones, and thus would reduce wound complication rates and chance of infection (6). While these potential complications do warrant concern, the results of our current meta-analysis show both MS and MT are safe and efficacious approaches for AVR with similar complication profiles.
While other outcomes are not well reported by the included studies and thus not available for Bayesian analysis, they must still be considered and factored when making the clinical decision to opt for a MS or MT approach. Firstly, the MS approach involves splitting the sternum, often in one or two directions. Consequently, a greater amount of time is required for the sternum to heal, and this may potentially prolong hospitalization (6). With a sternal incision, even if it is smaller, the time required for the bone to heal also means that restrictions are imposed on patients for a period following the operation to avoid excess mechanical stress. While proponents of MS suggest that MT may be associated with more pain, due to stretching of intercostal nerves (32), muscles and parietal pleura, the ease of delivering intercostal nerve block must also be considered. Given the complex learning curve and the apparent evidence of equivalent safety in MS and MT, it seems the best approach is one that is individualized not only to the patient but also to the technical skill and experience of the heart team involved.
Limitations
The present network meta-analysis has several constraints. Firstly, Bayesian analysis could not be performed on all outcomes including intensive care stay, hospitalization length and pain scoring, due to incomplete or inconsistent reporting of outcomes. Other relevant patient outcome measures including quality of life scores and cost-effectiveness economic analyses were rarely carried out. As such, these outcomes could not be compared between MS, MT and CS approaches for MIAVR. Secondly, there were no randomized or propensity-matched studies that directly compared MS and MT approaches. As such, inconsistency could not be statistically assessed using node-splitting methods. To maximize exchangeability of the included studies, carefully chosen randomized and propensity-matched trials were included with matched baseline characteristics. The more conservative results obtained using an inconsistency model, as opposed to a consistency model, were also presented. Despite these measures there was still significant heterogeneity detected in the operative parameters including CPB and cross-clamp duration, which may be due to different patient cohort characteristics and selection criteria among the studies. The heterogeneity may also reflect the variation in experience and expertise of different centers, given that MIAVR is associated with a significant learning curve. Thirdly, although mortality and morbidity outcomes were favorable in the short term, there is a shortage of robust long term clinical data.
Future adequately powered, prospective studies directly comparing MS and MT with consistent and complete reporting will be necessary to inform future policies and evidenced-based guidelines. Additionally, collaborative pooling of individual patient data, propensity-matched analyses and adequately powered randomized studies will assist in patient selection, risk stratification and prognosis. Multi-institutional registries and prospective studies investigating sutureless AVR, overseen by the International Valvular Surgery Study Group (IVSSG), have great potential to overcome the limitations of smaller sized observational studies.
Conclusions
The current evidence demonstrates that MIAVR via MS or MT is a safe and efficacious alternative to CAVR. Traditional and Bayesian analyses were consistent and did not yield any statistical differences between MS and MT approaches, except for longer CPB and cross-clamp durations with MT. Continual improvements in the long term safety and efficacy of sutureless valve technology may facilitate elimination of such differences in operative times. An individualized approach tailored to both the patient and surgical team is recommended for optimal outcomes.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Murtuza B, Pepper JR, Stanbridge RD, et al. Minimal access aortic valve replacement: is it worth it? Ann Thorac Surg 2008;85:1121-31. [PubMed]
- Phan K, Xie A, Di Eusanio M, et al. A Meta-Analysis of Minimally Invasive Versus Conventional Sternotomy for Aortic Valve Replacement. Ann Thorac Surg 2014;98:1499-511. [PubMed]
- Glauber M, Miceli A, Bevilacqua S, et al. Minimally invasive aortic valve replacement via right anterior minithoracotomy: early outcomes and midterm follow-up. J Thorac Cardiovasc Surg 2011;142:1577-9. [PubMed]
- Glauber M, Miceli A, Gilmanov D, et al. Right anterior minithoracotomy versus conventional aortic valve replacement: a propensity score matched study. J Thorac Cardiovasc Surg 2013;145:1222-6. [PubMed]
- Glower DD, Desai BS, Hughes GC, et al. Aortic valve replacement via right minithoracotomy versus median sternotomy: a propensity score analysis. Innovations (Phila) 2014 ;9:75-81; discussion 81.
- Brown ML, McKellar SH, Sundt TM, et al. Ministernotomy versus conventional sternotomy for aortic valve replacement: a systematic review and meta-analysis. J Thorac Cardiovasc Surg 2009;137:670-679.e5.
- Calderon J, Richebe P, Guibaud JP, et al. Prospective randomized study of early pulmonary evaluation of patients scheduled for aortic valve surgery performed by ministernotomy or total median sternotomy. J Cardiothorac Vasc Anesth 2009;23:795-801. [PubMed]
- Moustafa MA, Abdelsamad AA, Zakaria G, et al. Minimal vs median sternotomy for aortic valve replacement. Asian Cardiovasc Thorac Ann 2007;15:472-5. [PubMed]
- Ak K, Aybek T, Wimmer-Greinecker G, et al. Evolution of surgical techniques for atrial septal defect repair in adults: a 10-year single-institution experience. J Thorac Cardiovasc Surg 2007;134:757-64. [PubMed]
- Bonacchi M, Prifti E, Giunti G, et al. Does ministernotomy improve postoperative outcome in aortic valve operation? A prospective randomized study. Ann Thorac Surg 2002;73:460-5; discussion 465-6. [PubMed]
- Jansen JP, Crawford B, Bergman G, et al. Bayesian meta-analysis of multiple treatment comparisons: an introduction to mixed treatment comparisons. Value Health 2008;11:956-64. [PubMed]
- Ades AE, Sculpher M, Sutton A, et al. Bayesian methods for evidence synthesis in cost-effectiveness analysis. Pharmacoeconomics 2006;24:1-19. [PubMed]
- Caldwell DM, Ades AE, Higgins JP. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ 2005;331:897-900. [PubMed]
- Ahangar AG, Charag AH, Wani ML, et al. Comparing Aortic Valve Replacement through Right Anterolateral Thoracotomy with Median Sternotomy. Int Cardiovasc Res J 2013;7:90-4. [PubMed]
- Dogan S, Dzemali O, Wimmer-Greinecker G, et al. Minimally invasive versus conventional aortic valve replacement: a prospective randomized trial. J Heart Valve Dis 2003;12:76-80. [PubMed]
- Mächler HE, Bergmann P, Anelli-Monti M, et al. Minimally invasive versus conventional aortic valve operations: a prospective study in 120 patients. Ann Thorac Surg 1999;67:1001-5. [PubMed]
- Aris A, Cámara ML, Montiel J, et al. Ministernotomy versus median sternotomy for aortic valve replacement: a prospective, randomized study. Ann Thorac Surg 1999;67:1583-7; discussion 1587-8. [PubMed]
- Merk DR, Lehmann S, Holzhey DM, et al. Minimal invasive aortic valve replacement surgery is associated with improved survival: a propensity-matched comparison. Eur J Cardiothorac Surg 2014. [Epub ahead of print]. [PubMed]
- Furukawa N, Kuss O, Aboud A, et al. Ministernotomy versus conventional sternotomy for aortic valve replacement: matched propensity score analysis of 808 patients. Eur J Cardiothorac Surg 2014;46:221-6; discussion 226-7. [PubMed]
- Gilmanov D, Bevilacqua S, Murzi M, et al. Minimally invasive and conventional aortic valve replacement: a propensity score analysis. Ann Thorac Surg 2013;96:837-43. [PubMed]
- Bang JH, Kim JW, Lee JW, et al. Minimally invasive approaches versus conventional sternotomy for aortic valve replacement: a propensity score matching study. Korean J Thorac Cardiovasc Surg 2012;45:80-4. [PubMed]
- Johnston DR, Atik FA, Rajeswaran J, et al. Outcomes of less invasive J-incision approach to aortic valve surgery. J Thorac Cardiovasc Surg 2012;144:852-858.e3.
- Ruttmann E, Gilhofer TS, Ulmer H, et al. Propensity score-matched analysis of aortic valve replacement by mini-thoracotomy. J Heart Valve Dis 2010;19:606-14. [PubMed]
- Tabata M, Aranki SF, Fox JA, et al. Minimally invasive aortic valve replacement in left ventricular dysfunction. Asian Cardiovasc Thorac Ann 2007;15:225-8. [PubMed]
- Sharony R, Grossi EA, Saunders PC, et al. Propensity score analysis of a six-year experience with minimally invasive isolated aortic valve replacement. J Heart Valve Dis 2004;13:887-93. [PubMed]
- Neely RC, Boskovski MT, Gosev I, et al. Mini AVR versus AVR through full sternotomy; Harvard Medical School, The Brigham and Women’s Hospital experience. Ann Cardiothorac Surg 2014. [Epub ahead of print].
- Miceli A, Murzi M, Gilmanov D, et al. Minimally invasive aortic valve replacement using right minithoracotomy is associated with better outcomes than ministernotomy. J Thorac Cardiovasc Surg 2014;148:133-7. [PubMed]
- Phan K, Tsai YC, Niranjan N, et al. Sutureless aortic valve replacement: a systematic review and meta-analysis. Ann Cardiothorac Surg 2014. [Epub ahead of print].
- Modi P, Chitwood WR Jr. Retrograde femoral arterial perfusion and stroke risk during minimally invasive mitral valve surgery: is there cause for concern? Ann Cardiothorac Surg 2013;2:E1. [PubMed]
- Murzi M, Cerillo AG, Miceli A, et al. Antegrade and retrograde arterial perfusion strategy in minimally invasive mitral-valve surgery: a propensity score analysis on 1280 patients. Eur J Cardiothorac Surg 2013;43:e167-72. [PubMed]
- LaPietra A, Santana O, Mihos CG, et al. Incidence of cerebrovascular accidents in patients undergoing minimally invasive valve surgery. J Thorac Cardiovasc Surg 2014;148:156-60. [PubMed]
- Trehan N, Malhotra R, Mishra Y, et al. Comparison of ministernotomy with minithoracotomy regarding postoperative pain and internal mammary artery characteristics. Heart Surg Forum 2000;3:300-6. [PubMed]





