Role of entry tear size in type B aortic dissection
The long-term evolution of type B aortic dissection (AD) is associated with relatively high mortality and/or need for surgery, approaching 50% in 5 years (1). Some clinical predictive factors such as age, chronic obstructive pulmonary disease, systemic hypertension and Marfan syndrome have been associated with a high risk of complications. However, information obtained by imaging techniques has provided significant prognostic value. In addition to maximum aortic diameter, false lumen diameter (>22 mm) at the upper descending thoracic aorta level (2) or partial false lumen thrombosis have been associated with a higher risk of mortality and aortic dilatation (3).
Aim and methods
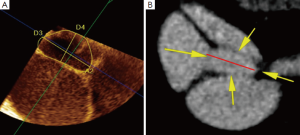
With the aim of defining the imaging variables obtained in the subacute phase that could predict adverse events during follow-up, we studied 184 consecutive patients: 108 surgically-treated type A and 76 medically-treated type B, discharged after an acute AD with patent false lumen (4). Trans-esophageal echocardiography (TEE) or computed tomography (CT) was performed prior to discharge. The following imaging variables were pre-specified and carefully assessed at each examination: (I) maximum aortic diameter in the ascending aorta, arch and descending aorta segments determined by CT; (II) antegrade or retrograde false lumen flow analyzed by contrast CT; (III) true lumen compression considered to be present when true lumen diameter represented less than 25% of the overall aortic diameter in axial slices by imaging tests, at least along two-thirds of the length of the descending thoracic aorta; and (IV) entry tear or main proximal communication between true and false lumina defined as the largest communication causing maximum entry flow into the patent false lumen. Entry tear size was quantified by the maximum diameter of the tear by TEE using longitudinal and transverse views or by CT (Figure 1). Patients were discharged with beta-blocker treatment, if not contraindicated, and may or may not be combined with other antihypertensive drugs aimed at achieving systolic blood pressure <130 mmHg. Imaging tests (CT, TEE or MRI depending on medical criteria) were performed at three and six months and annually thereafter.
Results
Entry tear size ranged from 3 to 26 mm (median: 7 mm; IQR: 5-12 mm). Entry tear size was larger in type B than in type A dissections (10.4±5.2 vs. 7.3±4.2 mm; P<0.001). Entry tear diameter was ≥10 mm in 45 (59.2%) of type B and in only 31 (40.8%) of operated type A dissections (P<0.001). The frequency of true lumen compression was similar in both types.
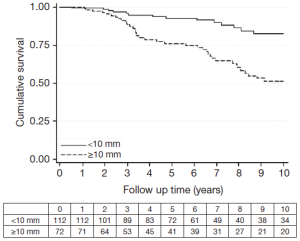
Median follow-up was 6.4 years (range, 0.5-17 years; IQR: 3.3-10.5 years). Seven patients underwent surgical and 28 endovascular treatment (10 patients with type A and 25 patients with type B AD) due to severe aortic dilatation, impending rupture and/or peripheral ischemia. Forty-nine patients died during follow-up (22 type A, 27 type B). Of these, 31 died suddenly: 11 during readmission with signs of aortic rupture and 20 at home from unknown causes. Six hospitalized patients died during surgical (n=3) or endovascular (n=3) treatment performed for chest pain and severe aortic dilatation. The remaining 12 patients died from causes not directly related to AD. Survival free from sudden death or surgical/endovascular treatment for the total population at 3, 5 and 10 years was 0.90 (95% CI, 0.84-0.94), 0.81 (95% CI, 0.75-0.87) and 0.46 (95% CI, 0.36-0.55), respectively. Patients with entry tear size ≥10 mm experienced a higher incidence of dissection-related events than those with entry tear <10 mm [HR =5.8; 95% CI, 3.3-10; P<0.001]. The median growth rate in patients with entry tear ≥10 mm was significantly higher than in patients with an entry tear <10 mm (0.80 mm, IQR: 0.17-1.88 vs. 0.16 mm, IQR: 0.07-0.48, P<0.001, respectively) (Figure 2). Multivariable predictors of events were Marfan syndrome, baseline maximum descending aortic diameter and entry tear size. Entry tear diameter ≥10 mm, when located in the proximal part of the dissection, conferred the poorest prognosis.
Limitations
Although maximum entry tear diameter may not be representative of entry tear size, this parameter showed good reproducibility both by TEE and CT. Maximum entry tear diameter measured by 3D-TEE showed a better correlation with CT than 2D-TEE (0.96 and 0.87, P=0.001, respectively) (5). Entry tear area measured by 3D-TEE and CT showed the best correlation (r=0.97) and agreement (0.05+0.20 cm2, P>0.05). In our series, an entry tear area of 1 cm2 was the value which corresponded to the maximum entry tear diameter of 10 mm (5). However, the predictive value of this parameter should be validated in other series.
Discussion
Although the short-term evolution after the acute phase of AD is stable, the incidence of complications rises after three years. Surgical or endovascular entry tear closure promotes both thrombosis of the false lumen and remodelling of the entire aorta. It has been suggested that the efficacy of these treatments is better in the subacute phase than in subsequent periods when the aorta is severely dilated and the intima is less elastic. Our findings may help to identify patients at higher risk of complications by using imaging techniques performed in the subacute phase of AD. In addition to a dilated aorta, the clinical outcome is more likely to be poorer in those with large entry tears. Thus, these patients may benefit from more aggressive surveillance and treatment. Experimental studies have shown that a large entry tear and inadequate outflow from the false lumen may lead to a significant increase in mean arterial and diastolic pressure from the false lumen (6).
Clinical bottom-line
In addition to Marfan syndrome, maximum aortic diameter and the presence of a large entry tear confer higher incidence of complications during follow-up. Information obtained by imaging techniques in the subacute phase can help to identify a high-risk subgroup of patients who may benefit from earlier and more aggressive therapy, including surgery or endovascular treatment, to improve their long-term prognosis.
Acknowledgements
Funding: Supported by grants from the Fondo de Investigación Sanitaria, Red de Investigación Cooperativa de las Enfermedades Cardiovasculares from the Instituto de Salud Carlos III, Ministerio de Sanidad y Consumo, and from the Sociedad Española de Cardiologia.
Disclosure: The authors declare no conflict of interest.
References
- Estrera AL, Miller CC 3rd, Safi HJ, et al. Outcomes of medical management of acute type B aortic dissection. Circulation 2006;114:I384-9. [PubMed]
- Song JM, Kim SD, Kim JH, et al. Long-term predictors of descending aorta aneurysmal change in patients with aortic dissection. J Am Coll Cardiol 2007;50:799-804. [PubMed]
- Tsai TT, Evangelista A, Nienaber CA, et al. Partial thrombosis of the false lumen in patients with acute type B aortic dissection. N Engl J Med 2007;357:349-59. [PubMed]
- Evangelista A, Salas A, Ribera A, et al. Long-term outcome of aortic dissection with patent false lumen: predictive role of entry tear size and location. Circulation 2012;125:3133-41. [PubMed]
- Evangelista A, Aguilar R, Cuellar H, et al. Usefulness of real-time three-dimensional transoesophageal echocardiography in the assessment of chronic aortic dissection. Eur J Echocardiogr 2011;12:272-7. [PubMed]
- Rudenick PA, Bijnens BH, García-Dorado D, et al. An in vitro phantom study on the influence of tear size and configuration on the hemodynamics of the lumina in chronic type B aortic dissections. J Vasc Surg 2013;57:464-474.e5.





