A meta-analysis of minimally invasive versus conventional mitral valve repair for patients with degenerative mitral disease
Abstract
Background: Minimally invasive mitral valve surgery through a mini-thoracotomy approach was developed in the mid-1990s as an alternative to conventional sternotomy, but with reduced trauma and quicker recovery. However, technical demands and a paucity of comparative data have thus far limited the widespread adoption of minimally invasive mitral valve repair (MIMVR). Previous meta-analyses have grouped various surgical techniques and underlying valvular disease aetiologies together for comparison. The present study aimed to compare the clinical outcomes of MIMVR versus conventional mitral valve repair in patients with degenerative mitral valve disease.
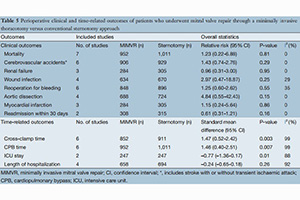
Methods: A systematic review of the current literature was performed through nine electronic databases from January 1995 to July 2013 to identify all relevant studies with comparative data on MIMVR versus conventional mitral valve surgery. Measured endpoints included mortality, stroke, renal failure, wound infection, reoperation for bleeding, aortic dissection, myocardial infarction, atrial fibrillation, readmission within 30 days, cross clamp time, cardiopulmonary bypass time and durations of intensive care unit (ICU) stay and overall hospitalization. Echocardiographic outcomes were also assessed when possible.
Results: Seven relevant studies were identified according to the predefined study selection criteria, including one randomized controlled trial and six retrospective studies. Meta-analysis of clinical outcomes did not identify any statistically significant differences between MIMVR and conventional mitral valve repair. The duration of ICU stay was significantly shorter for patients who underwent MIMVR, but this did not translate to a shorter hospitalization period. Patients who underwent MIMVR required longer cross clamp time as well as cardiopulmonary bypass time. Both surgical techniques appeared to achieve satisfactory echocardiographic outcomes. Pain-related outcomes was assessed in one study and reported significantly less pain for patients who underwent MIMVR. However, this limited data was not suitable for meta-analysis.
Conclusions: The existing literature has limited data on comparative outcomes after MIMVR versus conventional mitral valve repair for patients with degenerative disease. From the available evidence, there are no significant differences between the two surgical techniques in regards to clinical outcomes. Patients who underwent MIMVR required longer cardiopulmonary bypass and cross clamp times, but the duration of stay in the ICU was significantly shorter than conventional mitral valve repair.
Cover