A systematic review and meta-analysis on the safety and efficacy of the frozen elephant trunk technique in aortic arch surgery
Introduction
Surgical management of extensive arch pathologies involving the ascending aorta, aortic arch, and the descending aorta remains a complex and challenging operation. The unique anatomy of the arch and descending aorta demands special attention to minimize complications to brain and distal organ function, particularly in individuals with an aneurysm or dissection that involves the aortic arch and extends to the proximal descending aorta.
The introduction of the elephant trunk technique by Borst and colleagues in 1983 promoted staged surgical repair of arch and distal aortic aneurysms (1). By extending a graft from the distal aortic arch into the proximal descending aorta (which gives rise to the eponymous ‘elephant trunk’ appearance), repair of descending aortic pathologies can be more easily accomplished either through a second-stage lateral thoracotomy or by using it as a proximal landing zone for endovascular stenting. While such a strategy reduces the aortic occlusion time required for proximal anastomosis, its effectiveness is limited by significant cumulative operative mortality and interval mortality—often related to protracted duration between stages—and patients’ failure to return for second-stage completion operations (2,3).
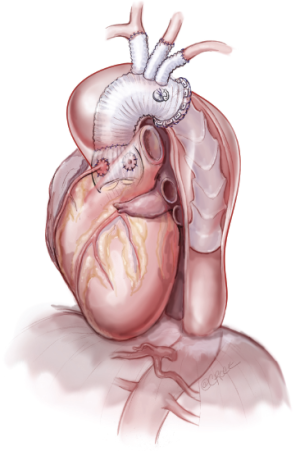
In the 1990s, development of new elephant trunk prostheses facilitated the treatment of aortic arch and proximal descending pathologies in a single operation while also minimizing complications associated with the conventional elephant trunk (4). These hybrid stent-graft prostheses encompass a covered stent sutured to the distal end of a conventional tube graft to provide expansive radial force on the distal portion of the elephant trunk (Figure 1). Similarly, some centers also prefer to deploy a conventional endovascular stent distal to the arch graft under direct vision instead of using a prefabricated prosthesis. Regardless, the combination of conventional surgery with endovascular techniques minimizes the need for a second procedure, while limiting residual patency of the false lumen and encouraging aortic wall remodeling (5,6).
The rapid advancements in prosthesis design and surgical strategies for distal arch and proximal descending aortic pathologies necessitate a contemporary appraisal. The present systematic review and meta-analysis evaluates the latest evidence regarding the safety and efficacy of this approach.
Methods
Literature search strategy
Electronic searches were performed using Ovid Medline, PubMed, Cochrane Central Register of Controlled Trials (CCTR), Cochrane Database of Systematic Reviews (CDSR), ACP Journal Club, and Database of Abstracts of Review of Effectiveness (DARE) from their date of inception to June 2013. To achieve the maximum sensitivity of the search strategy and identify all studies, we combined the terms: “frozen elephant trunk (FET)” OR “stented elephant trunk” OR “antegrade stenting descending thoracic aorta” as either key words or MeSH terms. The reference lists of all retrieved articles were reviewed for further identification of potentially relevant studies. All identified articles were systematically assessed using the inclusion and exclusion criteria.
Selection criteria
Eligible studies for the present systematic review and meta-analysis included those in which patient cohorts underwent surgery for aortic arch and descending arch pathologies, which utilized the FET approach. Studies that did not include predetermined primary or secondary endpoints were excluded. When institutions published duplicate studies with accumulating numbers of patients or increased lengths of follow-up, only the most complete reports were included for quantitative assessment at each time interval. All publications were limited to those involving human subjects and in the English language. Abstracts, case reports, conference presentations, editorials, and expert opinions were excluded. Review articles were omitted because of potential publication bias and duplication of results.
Data extraction and critical appraisal
All data were extracted from article texts, tables and figures by one of the investigators (B.W.). Data was subsequently reviewed and tabulated by another investigator (D.H.T.). Discrepancies between the two reviewers were resolved by discussion and consensus. The final results were reviewed by the senior investigator (T.D.Y.). The quality of studies was assessed using criteria recommended by the National Health Service Centre for Reviews and Dissemination case series quality assessment criteria (University of York, Heslington, United Kingdom) (7). Data are presented as mean ± standard deviation. Weighted means are calculated by determining the total number of events divided by total sample size. Weighted Spearman’s coefficient (rs) is used to calculate correlation between non-parametric continuous variables using SPSS version 21 (SPSS Inc, Chicago, USA). A significant P value is assumed to be
Results
Quality of studies
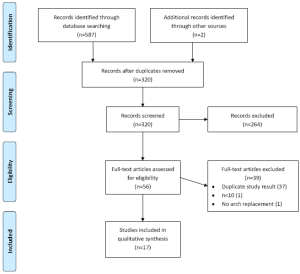
A total of 587 studies were identified through 6 electronic database searches (Figure 2). After exclusion of duplicate or irrelevant references, 55 potentially relevant articles were retrieved. After detailed evaluation of these articles, 15 studies remained for assessment. A manual search of reference lists yielded one new study. Another study published after the initial literature search was identified by the senior author, and was judged to be worthy of inclusion.
All of the included studies were retrospective observational studies (Level 4 evidence) (6,8-22), with only one prospective series (23). Seven series had >50 patients (range, 122-398 patients) (10,11,14,15,19-21), including a multi-centered registry (n=274) (15), while the remaining 10 studies had less than 50 patients (range, 17-46 patients) (6,8,9,11,12,16-18,22,23). Thirteen studies defined dissections according to the Stanford system (6,8,10,12,14-23), while the remainder utilized the DeBakey system (9,11,13,22), of which all but one was for DeBakey Type I dissections. Criteria for use of FET were stated in 5 studies (8-10,14,18), and included aortic diseases extending past the distal aorta (8,10,14,15), redo surgery (9,10), or other protocols (9,10). The prospective series enrolled all consecutive patients with acute type A aortic dissection aged 25-70 years (23). Two other studies relied upon surgeon’s preference (11,12). No indication of the representativeness of the sample was stated in any studies.
Five studies reported follow-up of greater than 3 years (range, 42-65 months) (10,12,14,18,19). Eight studies had follow-up less than 3 years (range, 12-35 months) (6,8,9,11,13,16,17,23), while the remaining studies did not report length of follow-up (15,20-22). Survival at 1-year, 3-year, and 5-year was reported by 7 studies (8,10,15,17-19,21), 4 studies (10,15,18,21), and 5 studies (10,13,15,18,19), respectively. Two studies reported survival beyond 5 years (10,19).
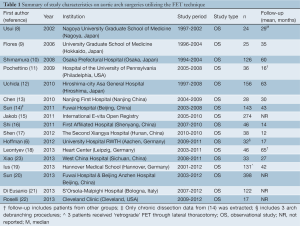
The study characteristics are summarized in Table 1. In these 17 studies, 1,675 patients underwent procedures that involved either a frozen or stented elephant trunk.
Full table
Demographic and operative characteristics
Overall, 77.2% of patients were male, with a weighted mean age of 56.5±13.4 years old. Surgical indication was exclusively type A acute dissection in 7 studies (6,11,16,17,20,22,23), while the rest included a combination of acute and chronic type A and type B dissections and aneurysms. Overall, indication was type A acute and chronic dissection in 51.9% and 21.1% of all patients, respectively, and type B acute and chronic dissection in 2.4% and 3.1%, respectively. Aneurysms were the indication for 19.1% of all patients. Marfan’s syndrome was present in 8.6% of patients (range, 2.4-21.2%) in 10 studies (6,10,13-17,19,20,23), while preoperative renal insufficiency/failure was reported in all but two studies (8,17) with a weighted average prevalence of 8.6% (range, 0-20.5%). Other patient demographics reported by more than half of the studies included hypertension, coronary artery disease, cerebral vasculopathies, diabetes, chronic obstructive pulmonary disease, and previous cardiac surgery.
A variety of prefabricated and modified prostheses were utilized (Table 2) by these centers. Aortic valve repair/replacement, Bentall procedure, and coronary artery bypass grafting was performed in 14.7%, 20.0% and 11.9%, respectively, in studies which specifically reported these procedures.

Full table
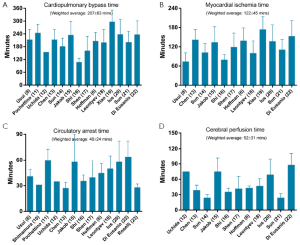
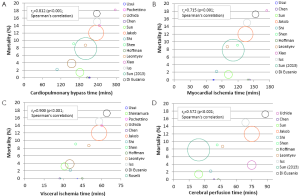
Weighted average cardiopulmonary bypass time, myocardial ischemic time, circulatory arrest time, and cerebral perfusion time were 207±63 minutes (range, 108-297 minutes), 122±45 minutes (range, 74-174 minutes), 48±24 minutes (range, 27.2-64 minutes), 52±31 minutes (range, 24-88 minutes), respectively (Figure 3). Significant strong positive linear relationships between mortality and cardiopulmonary bypass time (Spearman’s correlation coefficient, rs =0.812), circulatory arrest time (rs =0.715), and cerebral perfusion time (rs =0.900) were identified, respectively (Figure 4). Moderate positive linear relationships between mortality and myocardial ischemia time (rs =0.572), and between circulatory arrest time and incidence of spinal cord injury (rs =0.474), were identified.
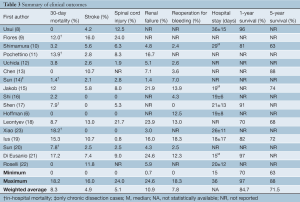
Assessment of safety
Six studies reported in-hospital mortality (9,11,14,17,20,23), while the remainder reported 30-day mortality (Table 3). Overall, average weighted mortality was 8.3% (range, 0-18.2%). Multiple organ failure was the most frequent cause of death, accounting for 51.3% of all deaths when details were provided. For studies that only included acute type A dissection, overall mortality was 7.7% (range, 0-18.2%).
Full table
Stroke was reported in all but one study (17), while spinal cord injury was reported in all but two studies (13,22). Postoperative stroke occurred in 4.9% of patients (range, 0-16%), while spinal cord injury was identified in 5.1% of patients (range, 0-24%). For studies examining acute type A dissection, stroke and spinal cord injury were identified in 2.2% (range, 0-11.8%) and 2.6% (range, 0-8.3%).
Thirteen studies reported data on postoperative renal failure, with a prevalence of 10.9% (1.4-24.6%), while reoperation for bleeding ranged between 0-18.3%. Hospital stay ranged between 15-36 days. Of the acute type A dissection studies, 4 reported results for postoperative renal failure and reoperation for bleeding at 5.2% and 3.1%, respectively.
Assessment of efficacy
Weighted 1-year survival was 85.6% (range, 70-97%) (10,17-19,21,24). 5-year survival was 71.5% (range, 63-88%), which was reported by 5 studies (10,13,15,18,19). No data was available from the included studies regarding cost-effectiveness and quality-of-life.
Discussion
The classic elephant trunk technique represents an evolutionary leap in the treatment of patients with extensive disease of the thoracic aorta, and has been recognized as the standard for the treatment of extended aortic pathologies involving the arch and descending aorta (1). However, recent studies have raised elements of concern regarding this procedure, including the cumulative and interval mortality, and the high failure rate of complete treatment (25-29). These elements have triggered further progress in surgical approaches, in particular, a growing uptake in hybrid operations, such as the FET technique.
The FET is a modification of the classic elephant trunk technique. By employing a stent-graft during conventional open arch repair, the distal stented portion of this prosthesis is able to provide a virtual anastomotic seal at the descending aorta. While this approach was initially designed to avoid second-stage completion operations following the classic elephant trunk procedure, its indications were expanded to patients with acute dissections and multi-segmental aneurysms (such as mega-aortic syndrome) (19). The reported advantages of the radial expansion of the stent-graft for aneurysmal disease include a single-stage curative treatment of arch aneurysms extending (and limited) to the proximal descending aorta, more effective prevention of anastomotic leakages, and reduction of the risk of kinking and flapping of the prosthesis. In terms of its use in aortic dissection, the stent-graft is able to seal descending aorta tears with compression of the false lumen and expansion of the true lumen, prevent further dilation of the proximal descending aorta, and increase the patency of the graft in collapsed lumens, in both stented and non-stented aortic segments (5,12,19,30,31).
The present review found acceptable overall mortality and stroke rates to be 8.3% and 4.9%, respectively. The vast majority of deaths were related to multi-organ failure (51.5%). The mortality rate and rates of stroke and spinal cord injuries were also promising in patients with acute dissection. These results are not dissimilar to that of total arch replacement (32,33) and are in-line with several reviews of the hybrid approach, which reported mortality between 6.4% to 9.0%, and stroke between 4.6-6.2% (28,34,35).
Spinal cord injury is a potential concern in FET procedures. For example, the International E-vita Open Registry reported a spinal cord injury rate of 8.0% in 274 patients (15,36). Although paraparesis and paraplegia resolved partially in 40% of these cases, they remain noteworthy complications. Comparatively, in the present analysis, the overall prevalence of postoperative spinal cord injury was lower, at 5.1%, which may be partially attributed to institutional variations in the length of the FET, as some studies with higher complication rates have pointed to the occlusion of intercostal arteries as a cause (13,21). For example, Flores and associates found that the distal landing zone is an independent risk factor for paraplegia, and cautions against placing a landing zone distal to T7 (9), while others recommend placement of the distal landing zone of the stent proximal to T8 and T9 (13,37), or even T10 (38). Interestingly, research from the Mount Sinai group identified the number of segmental arteries sacrificed as the most powerful predictor of paraplegia risk (39). Sacrificing less than twelve pairs of segmental arteries (beginning in the upper thorax) was associated with a reduced risk of paralysis compared to those sacrificed distal to the upper thorax, or if more arteries were sacrificed. Based on these results, Hoffman and coworkers safely placed the distal landing zone of the stent-graft between T10-T12, with no reported temporary or permanent paraplegia amongst 32 patients (6). Collectively, these conflicting findings made the interpretation of the current clinical data difficult. Further research is warranted in terms of the safe extent of coverage in aneurysmal and acute and chronic dissections.
In the present review, the association between circulatory arrest temperature and spinal cord injury is less clear, although porcine studies have demonstrated that spinal cord ischemic tolerance may extend to 50 minutes at 32 °C and 90 minutes at 28 °C (40). A trend for increased risk of spinal cord injury have been noted in several observational studies which utilized higher temperatures during aortic arch surgery (41,42). It is plausible that although the operation duration and potential risk of bleeding might be reduced at warmer arrest temperatures, spinal and distal organ protection could be compromised. In addition, a moderate positive linear relationship between circulatory arrest time and spinal cord injury was identified in the present review, as it is possible the average circulatory arrest time did not exceed tolerance threshold. It also needs to be borne in mind that spinal cord ischemia is a clinical endpoint of the survivors. It is likely, although this cannot be proven, that the incidence of spinal cord ischemia is underestimated in these study cohorts, as some patients did not survive the operation and spinal cord ischemia was simply not diagnosed. This emphasizes the importance of reporting a composite clinical endpoint including mortality, permanent neurological deficits, and permanent spinal cord ischemia in future studies. Finally, it is also not clear in the current literature, whether monitoring of motor evoked potential and spinal fluid drainage is indicated.
The present findings are limited by several key constraints. Firstly, all the studies were retrospective observational trials and significant variations in several critical surgical parameters have lessened the general applicability of the results. Secondly, outcomes were unable to be stratified according to underlying pathologies. Thirdly, several specially designed FET prostheses have not yet attained FDA approval in the United States, therefore introducing potential geographical confounders into the analysis. Some of these prostheses also simplify the anastomosis of the supra-aortic vessels and distal aortic stump, therefore reducing circulatory arrest time and minimizing the risk of associated complications (19). Finally, although 5-year survival is favorable at 71.5%, this was only present in 5 studies, and more long-term data are required. The shortage of long-term data beyond 5 years and the absence of randomized controlled trials comparing the FET technique with other hybrid approaches in similar patient cohorts limit the provision of evidence-based guidelines and recommendations. Long-term studies are also required to compare freedom from reoperations between FET and classic ET/staged approaches, particularly in the setting of acute dissection, as the former favors aortic remodeling.
In summary, FET provides the possibility of a single stage operation addressing distal arch and proximal descending aortic pathologies. Compared to the staged approach, it has obvious theoretical advantages. The main findings from the present systematic review and meta-analysis indicate that FET can be performed with acceptable mortality and morbidity in specialist centers. The potential risk of postoperative spinal cord ischemia needs to be evaluated further prior to widespread clinical use. Finally, the survival benefit, cost-effectiveness and quality of life improvement could not be ascertained without long-term comparative data.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Borst HG, Walterbusch G, Schaps D. Extensive aortic replacement using “elephant trunk” prosthesis. Thorac Cardiovasc Surg 1983;31:37-40. [PubMed]
- Heinemann MK, Buehner B, Jurmann MJ, et al. Use of the “elephant trunk Technique” in aortic surgery. Ann Thorac Surg 1995;60:2-6; discussion 7. [PubMed]
- Estrera AL, Miller CC 3rd, Porat EE, et al. Staged repair of extensive aortic aneurysms. Ann Thorac Surg 2002;74:S1803-5; discussion S1825-32.
- Kato M, Ohnishi K, Kaneko M, et al. New graft-implanting method for thoracic aortic aneurysm or dissection with a stented graft. Circulation 1996;94:II188-93. [PubMed]
- Baraki H, Hagl C, Khaladj N, et al. The frozen elephant trunk technique for treatment of thoracic aortic aneurysms. Ann Thorac Surg 2007;83:S819-23; discussion S824-31.
- Hoffman A, Damberg AL, Schälte G, et al. Thoracic stent graft sizing for frozen elephant trunk repair in acute type A dissection. J Thorac Cardiovasc Surg 2013;145:964-9. [PubMed]
- Reviews NCf, Dissemination. Undertaking systematic reviews of research on effectiveness: CRD’s guidance for those carrying out or commissioning reviews. CRD Report 4. 2001.
- Usui A, Fujimoto K, Ishiguchi T, et al. Cerebrospinal dysfunction after endovascular stent-grafting via a median sternotomy: the frozen elephant trunk procedure. Ann Thorac Surg 2002;74:S1821-4; discussion S1825-32.
- Flores J, Kunihara T, Shiiya N, et al. Extensive deployment of the stented elephant trunk is associated with an increased risk of spinal cord injury. J Thorac Cardiovasc Surg 2006;131:336-42. [PubMed]
- Shimamura K, Kuratani T, Matsumiya G, et al. Long-term results of the open stent-grafting technique for extended aortic arch disease. J Thorac Cardiovasc Surg 2008;135:1261-9. [PubMed]
- Pochettino A, Brinkman WT, Moeller P, et al. Antegrade thoracic stent grafting during repair of acute DeBakey I dissection prevents development of thoracoabdominal aortic aneurysms. Ann Thorac Surg 2009;88:482-9; discussion 489-90. [PubMed]
- Uchida N, Katayama A, Tamura K, et al. Long-term results of the frozen elephant trunk technique for extended aortic arch disease. Eur J Cardiothorac Surg 2010;37:1338-45. [PubMed]
- Chen X, Huang F, Xu M, et al. The stented elephant trunk procedure combined total arch replacement for Debakey I aortic dissection: operative result and follow-up. Interact Cardiovasc Thorac Surg 2010;11:594-8. [PubMed]
- Sun L, Qi R, Zhu J, et al. Total arch replacement combined with stented elephant trunk implantation: a new “standard” therapy for type a dissection involving repair of the aortic arch? Circulation 2011;123:971-8. [PubMed]
- Jakob H, Tsagakis K, Pacini D, et al. The International E-vita Open Registry: data sets of 274 patients. J Cardiovasc Surg (Torino) 2011;52:717-23. [PubMed]
- Shi E, Gu T, Yu L, et al. Repair of Stanford type A aortic dissection with ascending aorta and hemiarch replacement combined with stent-graft elephant trunk technique by using innominate cannulation. J Thorac Cardiovasc Surg 2011;142:1458-63. [PubMed]
- Shen K, Tang H, Jing R, et al. Application of triple-branched stent graft for Stanford type A aortic dissection: potential risks. Eur J Cardiothorac Surg 2012;41:e12-7. [PubMed]
- Leontyev S, Borger MA, Etz CD, et al. Experience with the conventional and frozen elephant trunk techniques: a single-centre study. Eur J Cardiothorac Surg 2013. [Epub ahead of print]. [PubMed]
- Ius F, Fleissner F, Pichlmaier M, et al. Total aortic arch replacement with the frozen elephant trunk technique: 10-year follow-up single-centre experience. Eur J Cardiothorac Surg 2013. [Epub ahead of print]. [PubMed]
- Ma WG, Zheng J, Dong SB, et al. Sun’s procedure of total arch replacement using a tetrafurcated graft with stented elephant trunk implantation: analysis of early outcome in 398 patients with acute type A aortic dissection. Ann Cardiothorac Surg 2013;2:621-8.
- Di Eusanio M, Pantaleo A, Murana G, et al. Frozen elephant trunk—the Bologna’s experience. Ann Cardiothorac Surg 2013;2:597-605.
- Roselli EE, Rafael A, Soltesz EG, et al. Simplified frozen elephant trunk repair for acute DeBakey type I dissection. J Thorac Cardiovasc Surg 2013;145:S197-201. [PubMed]
- Xiao Z, Meng W, Zhu D, et al. Treatment strategies for left subclavian artery during total arch replacement combined with stented elephant trunk implantation. J Thorac Cardiovasc Surg 2013. [Epub ahead of print]. [PubMed]
- Usui A, Ueda Y, Akita T, et al. Mid-term results of an endovascular stent-graft by means of median sternotomy for distal aortic arch aneurysm. Artif Organs 2002;26:1044-9. [PubMed]
- Safi HJ, Miller CC 3rd, Estrera AL, et al. Staged repair of extensive aortic aneurysms: morbidity and mortality in the elephant trunk technique. Circulation 2001;104:2938-42. [PubMed]
- LeMaire SA, Carter SA, Coselli JS. The elephant trunk technique for staged repair of complex aneurysms of the entire thoracic aorta. Ann Thorac Surg 2006;81:1561-9. [PubMed]
- Safi HJ, Miller CC 3rd, Estrera AL, et al. Optimization of aortic arch replacement: two-stage approach. Ann Thorac Surg 2007;83:S815-8; discussion S824-31.
- Ius F, Hagl C, Haverich A, et al. Elephant trunk procedure 27 years after Borst: what remains and what is new? Eur J Cardiothorac Surg 2011;40:1-11. [PubMed]
- Svensson LG, Kim KH, Blackstone EH, et al. Elephant trunk procedure: newer indications and uses. Ann Thorac Surg 2004;78:109-16. [PubMed]
- Mizuno T, Toyama M, Tabuchi N, et al. Stented elephant trunk procedure combined with ascending aorta and arch replacement for acute type A aortic dissection. Eur J Cardiothorac Surg 2002;22:504-9. [PubMed]
- Di Eusanio M, Armaro A, Di Marco L, et al. Short- and midterm results after hybrid treatment of chronic aortic dissection with the frozen elephant trunk technique. Eur J Cardiothorac Surg 2011;40:875-80. [PubMed]
- Okita Y, Minatoya K, Tagusari O, et al. Prospective comparative study of brain protection in total aortic arch replacement: deep hypothermic circulatory arrest with retrograde cerebral perfusion or selective antegrade cerebral perfusion. Ann Thorac Surg 2001;72:72-9. [PubMed]
- Kazui T, Yamashita K, Washiyama N, et al. Aortic arch replacement using selective cerebral perfusion. Ann Thorac Surg 2007;83:S796-8; discussion S824-31.
- Cao P, De Rango P, Czerny M, et al. Systematic review of clinical outcomes in hybrid procedures for aortic arch dissections and other arch diseases. J Thorac Cardiovasc Surg 2012;144:1286-300, 1300.e1-2.
- Karck M, Kamiya H. Progress of the treatment for extended aortic aneurysms; is the frozen elephant trunk technique the next standard in the treatment of complex aortic disease including the arch? Eur J Cardiothorac Surg 2008;33:1007-13. [PubMed]
- Pacini D, Tsagakis K, Jakob H, et al. The frozen elephant trunk for the treatment of chronic dissection of the thoracic aorta: a multicenter experience. Ann Thorac Surg 2011;92:1663-70; discussion 1670.
- Ishihara H, Uchida N, Yamasaki C, et al. Extensive primary repair of the thoracic aorta in Stanford type A acute aortic dissection by means of a synthetic vascular graft with a self-expandable stent. J Thorac Cardiovasc Surg 2002;123:1035-40. [PubMed]
- Chavan A, Karck M, Hagl C, et al. Hybrid endograft for one-step treatment of multisegment disease of the thoracic aorta. J Vasc Interv Radiol 2005;16:823-9. [PubMed]
- Zoli S, Roder F, Etz CD, et al. Predicting the risk of paraplegia after thoracic and thoracoabdominal aneurysm repair. Ann Thorac Surg 2010;90:1237-44. [PubMed]
- Etz CD, Luehr M, Kari FA, et al. Selective cerebral perfusion at 28 degrees C--is the spinal cord safe? Eur J Cardiothorac Surg 2009;36:946-55. [PubMed]
- Minatoya K, Ogino H, Matsuda H, et al. Evolving selective cerebral perfusion for aortic arch replacement: high flow rate with moderate hypothermic circulatory arrest. Ann Thorac Surg 2008;86:1827-31. [PubMed]
- Kamiya H, Hagl C, Kropivnitskaya I, et al. The safety of moderate hypothermic lower body circulatory arrest with selective cerebral perfusion: a propensity score analysis. J Thorac Cardiovasc Surg 2007;133:501-9. [PubMed]