Arterial grafts: clinical classification and pharmacological management
Abstract
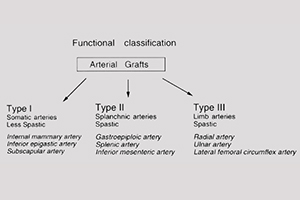
In comparison with standard saphenous vein grafts, use of the internal mammary artery (IMA) as a coronary artery bypass graft has achieved superior long-term results. This is related to the differences in the biological characteristics between the venous and arterial grafts. However, even arterial grafts are not uniform in their biological characteristics. The variation in the perioperative behavior of the grafts and in their long-term patency may be related to different characteristics. These factors should be taken into account in the use of arterial grafts, some of which are subjected to more active pharmacological intervention during and after the operation to obtain satisfactory results. To better understand the biological behavior of the grafts, their common features and their differences, a clinical classification may be useful for a practicing surgeon. Based on experimental studies of their vasoreactivity combined with anatomical, physiological and embryological considerations, we have proposed a functional classification for arterial grafts that may be useful clinically. Our classification suggests that there are three types of arterial grafts: Type I—somatic arteries; Type II— splanchnic arteries; and Type III—limb arteries. Type I arteries have enhanced endothelial function and release more nitric oxide and other relaxing factors. Type II arteries, such as the gastro-epiploic artery, and Type III arteries, such as the radial artery (RA), have higher pharmacological reactivity to vasoconstrictors. This classification explains why the IMA has the best long-term patency. Because Type II and III arteries are prone to spasms due to higher contractility, they require more active pharmacological interventions. Furthermore, the harvesting technique of the conduits, including the saphenous vein and IMA, are described and discussed in this article. Prevention of spasms using two cocktails of medications (verapamil + nitroglycerin and nicardipine + nitroglycerin) during harvesting of the conduits is described. These solutions have been demonstrated to be clinically effective.
Cover