Radial artery as a second arterial graft in the elderly and both sexes
Introduction
The left internal thoracic artery to left anterior descending (LITA-LAD) graft is the cornerstone of modern coronary artery bypass grafting (CABG) surgery. The favorable effect on long-term outcomes of using the LITA arterial conduit over saphenous vein for grafting is well established, and is attributed to superior durability of arterial grafts (1,2). Multiple groups have also compellingly demonstrated that additional arterial grafts may further improve late outcomes of CABG surgery (3-11). However, in the United States and many other countries, the use of multiple arterial grafts in primary CABG operations remains below 10%. This has been the case despite a lack of substantive evidence justifying the use of conventional LITA-LAD with additional vein grafting (ITA/SV).
Women and elderly patients have been particularly under-represented in the majority of, if not all, the reported CABG series with multiple arterial grafting. In the case of the elderly, it is suggested that their limited life expectancy precludes them from realizing the late benefits of multiple arterial grafts. The current report focuses on the findings of two recent studies investigating the long-term benefits of using the radial artery as a second arterial conduit (ITA/RA) versus the ITA/SV approach in the elderly (12) and across both sexes (13).
Patients and methods
The two studies (12,13) employed nearly identical methods with retrospective analysis of a prospectively collected cardiac surgery database, collected and reported in accordance with the STS National Database definitions and criteria.
Patients and coronary grafts
The patients in both studies were derived from the 1996-2007 primary, non-salvage CABG experience at Mercy Saint Vincent Medical Center of Toledo, Ohio, USA. All included subjects had ≥2 completed grafts including one ITA graft (>99% LITA-LAD). Patients with bilateral ITA, ITA-only grafts, or concomitant valve/aortic surgery were excluded. This retained 6,384 patients (69% vs. 31%, male/female) for analysis in the study by sex (13). From this baseline population, the elderly study further excluded patients younger than 70 years of age at the time of CABG, retaining 2,605 elderly subjects (12). Late mortality data were secured from the United States Social Security Death Index Database (February 2012; http://ssdi.genealogy.rootsweb.com). Details on surgical technique over the study period have been previously described (6,9,10,13).
Propensity score models and matching
In the elderly study, patients were first separated into septuagenarian (70-79 years) and octogenarian (≥80 years) sub-cohorts and, within each, subsequently subdivided to the ITA/RA and ITA/SV grafting groups (12). Similarly, for the study by sex, separate grafting groups were derived for male and female patients. In all four cases, ITA/RA and ITA/SV cohorts exhibited significant demographic and risk factor differences. To minimize confounding due to these differences, separate RA-use (treatment) propensity score matching was done to arrive at matched ITA/RA and ITA/SV groups (12,13).
Data analysis
Kaplan-Meier and Cox regression analyses were applied to assess sex-specific and elderly-specific 12-year survival risk ratios of ITA/RA vs. ITA/SV grafting. A P-value less than 0.05 was used to indicate significance.
Results
Operative death (in-hospital or within 30 days) was similar for ITA/RA and ITA/SV in men, women, septuagenarians and octogenarians. The ITA/RA grafting subcohort demonstrated superior long-term survival across all four CABG subpopulations studied. Detailed early and late survival results for each group follow.
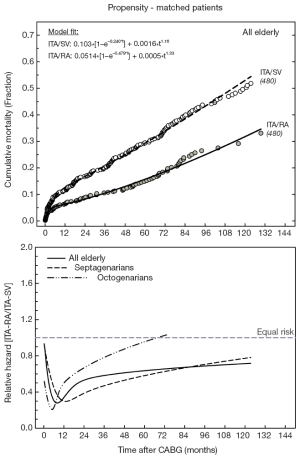
Elderly
In patients aged 70 years or older, operative death was essentially identical for ITA/RA vs. ITA/SV [14 of 607 (2.31%) vs. 35 of 1,513 (2.31%); P=0.880]. At late follow-up, total deaths were less frequent among ITA/RA vs. ITS/SV [118 of 607 (19.4%) vs. 577 of 1,513 (38.1%), respectively; P<0.001]. Unadjusted 12-year survival was significantly better for ITA/RA (overall; P<0.001), and this was true for both septuagenarians (P=0.003) and octogenarians (P=0.048). In 480 matched elderly pairs (79% of all ITA/RA), all patient factor differences were removed (standardized differences below 10%; P>0.2), resulting in identical operative mortality for ITA/RA and ITA/SV cohorts (both 2.3%). Cumulative mortality estimates at 1, 5 and 10 years remained substantially worse for ITA/SV for all elderly (P<0.001), and for septuagenarians (P<0.001) and octogenarians (P=0.032) separately (Figure 1). Cumulative mortality for the matched ITA/RA and ITA/SV cohorts exhibited biphasic (early and late) characteristics. Excluding all 30-day deaths, the risk ratio for ITA/RA versus ITA/SV grafting was 0.47 (95% confidence interval, 0.36-0.61), which is consistent with the relative hazard ratios versus time (Figure 1). These were essentially <1 (or less death risk for ITA/RA) for nearly the entire available follow-up time for all elderly patients and was qualitatively similar in septuagenarians and octogenarians.
By sex
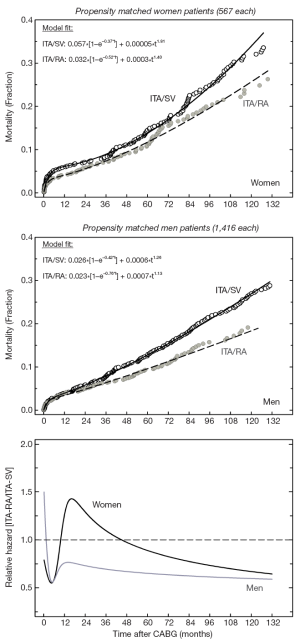
Operative death was similar in men and women [53/4,413 (1.20%) vs. 35/1,971 (1.78%); P=0.088] and, within each sex, operative mortality was similar for ITA/RA versus ITA/SV grafting [men: 19/1,946 (0.98%) vs. 34/2,467 (1.38%), P=0.281; women: 10/656 (1.52%) vs. 25/1,315 (1.90%), P=0.678]. Late mortality was significantly lower overall for ITA/RA versus ITA/SV in men (10.4% vs. 28.3%; P<0.001) and in women (13.6% vs. 28.5%; P<0.001). Subsequently, unadjusted 12-year survival was significantly better for ITA/RA versus ITA/SV, irrespective of gender (both P<0.001).
Matching resulted in 1,416 ITA/RA and ITA/SV matched pairs in men (73%) and 567 matched pairs in women (86%). All differences in demographic, co-morbidity, coronary disease and revascularization factors were removed after matching (all P>0.2; all standardized differences <10%). SV grafts were also used in matched male (80%) and female (77%) RA patients. For ITA/RA versus ITA/SV, operative mortality was similar in men [18/1,416 (1.28%) vs. 17/1,416 (1.20%); P=1.0] and women [8/567 (1.41%) vs. 11/567 (1.94%); P=0.644]. Alternatively, late mortality was significantly lower for ITA/RA subcohorts in both men [11.6% vs. 22.0%; P<0.001] and women (14.7% vs. 22.2%; P<0.001). The corresponding matched Kaplan-Meier cumulative mortality data were significantly better for ITA/RA irrespective of sex [men: RR=0.65 (0.54-0.79), P<0.001; women: RR=0.75 (0.57-0.99), P=0.045; Figure 2]. The comparatively more beneficial relative risks in males compared to female CABG patients were consistent with the relative hazard versus time data.
Discussion
These two studies indicate that ITA/RA is associated with improved long-term survival compared to the conventional ITA/SV approach, irrespective of sex (men and women) and elderly age overall, as well as for septuagenarians and octogenarians separately. Importantly, this is achieved without evidence of increased acute perioperative risk associated with utilization of the RA, a conduit that is often perceived as being more technically difficult to handle and which, given its documented advantages, remains inexplicably underutilized in contemporary practice in the United States (12,13).
The study of elderly patients aimed to objectively address the claim that the ITA/RA may not be warranted in elderly (>70 years) and very elderly (>80 years) CABG subgroups because the expected survival benefits of using RA grafts may not be realizable given reasonable life expectancy limits (12). Indeed, as the first elderly-specific analysis of ITA/RA grafting, it reported that the elderly overall, regardless of whether septuagenarian or older, experienced decreased cumulative risk adjusted (by propensity matching) long-term mortality. The magnitude of this multiple versus single arterial graft effect was a formidable 53% reduction in 12-year cumulative mortality.
The study by sex clarified the previously unexamined impact of ITA/RA grafting on long-term survival by sex. While improved long-term survival was associated with ITA/RA in men and women, the benefits manifested differently by sex, as evidenced by the hazard functions. In men, the benefit appears later when compared with women but is relatively greater and more consistent. In women, following an early 1-year survival advantage with RA use, there appears to be a relative disadvantage in survival between 12 and 36 months. In the long-term, the 12-year cumulative survival benefit conferred by the ITA/RA grafting approach relative to the ITA/SV is seen in both males and females with a relative reduction in mortality [derived as: 100%×(1–RR)] of 35% in males and 25% in females. A very recent study corroborated our data and found that women receiving ITA/RA had significant 15-year survival advantages over matched ITA/SV patients (14).
We speculate that the enhanced survival of ITA/RA groups is due to the at least equivalent and most likely improved long-term durability of the RA compared to the SV graft, as previously documented (6,9,13,15-17). A limitation of these studies is their retrospective, 11-year single institution experience with RA grafting and thus their conclusions may not be immediately generalizable. The latter is partially mitigated by other independent patient series analyses, which have shown improved late survival with multiple arterial grafts achieved by using the RA as a second arterial graft. Despite using propensity matching to minimize patient selection bias, these studies remain a retrospective analysis with the possibility of uncontrolled confounding effects. Furthermore, we are unable to unambiguously attribute the improved survival in the different groups to the effects of the RA, specifically to its presumed enhanced patency rates, as neither the cause of death nor graft patency data are available.
In conclusion, these two reports support more liberal use of the RA as a second arterial conduit instead of the SV in the elderly and irrespective of sex. Given the documented benefits of multiple arterial grafts in these two studies, as well as previous related reports, it is difficult to understand the tragically low utilization rate of multiple arterial conduits by cardiac surgeons today. We believe that in light of the compelling and growing data establishing superior patency of arterial grafts (16,17) and concurrent improved survival, it is time for our professional societies to establish multiple arterial grafting as a quality benchmark—paralleling the experience with rapid adoption of the LIMA to LAD graft as a standard of care.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Loop FD, Lytle BW, Cosgrove DM, et al. Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events. N Engl J Med 1986;314:1-6. [PubMed]
- Zeff RH, Kongtahworn C, Iannone LA, et al. Internal mammary artery versus saphenous vein graft to the left anterior descending coronary artery: prospective randomized study with 10-year follow-up. Ann Thorac Surg 1988;45:533-6. [PubMed]
- Lytle BW, Blackstone EH, Sabik JF, et al. The effect of bilateral internal thoracic artery grafting on survival during 20 postoperative years. Ann Thorac Surg 2004;78:2005-12; discussion 2012-4.
- Rankin JS, Tuttle RH, Wechsler AS, et al. Techniques and benefits of multiple internal mammary artery bypass at 20 years of follow-up. Ann Thorac Surg 2007;83:1008-14; discussion 1014-5. [PubMed]
- Kurlansky PA, Traad EA, Dorman MJ, et al. Thirty-year follow-up defines survival benefit for second internal mammary artery in propensity-matched groups. Ann Thorac Surg 2010;90:101-8. [PubMed]
- Zacharias A, Habib RH, Schwann TA, et al. Improved survival with radial artery versus vein conduits in coronary bypass surgery with left internal thoracic artery to left anterior descending artery grafting. Circulation 2004;109:1489-96. [PubMed]
- Lawton JS, Barner HB, Bailey MS, et al. Radial artery grafts in women: utilization and results. Ann Thorac Surg 2005;80:559-63. [PubMed]
- Tranbaugh RF, Dimitrova KR, Friedmann P, et al. Radial artery conduits improve long-term survival after coronary artery bypass grafting. Ann Thorac Surg 2010;90:1165-72. [PubMed]
- Schwann TA, Zacharias A, Riordan CJ, et al. Sequential radial artery grafts for multivessel coronary artery bypass graft surgery: 10-year survival and angiography results. Ann Thorac Surg 2009;88:31-9. [PubMed]
- Zacharias A, Schwann TA, Riordan CJ, et al. Late results of conventional versus all-arterial revascularization based on internal thoracic and radial artery grafting. Ann Thorac Surg 2009;87:19-26.e2.
- Zacharias A, Schwann TA, Riordan CJ, et al. Late outcomes after radial artery versus saphenous vein grafting during reoperative coronary artery bypass surgery. J Thorac Cardiovasc Surg 2010;139:1511-8.e4.
- Habib RH, Schwann TA, Engoren M. Late effects of radial artery versus saphenous vein grafting in patients aged 70 years or older. Ann Thorac Surg 2012;94:1478-84. [PubMed]
- Schwann TA, Engoren M, Bonnell M, et al. Comparison of late coronary artery bypass graft survival effects of radial artery versus saphenous vein grafting in male and female patients. Ann Thorac Surg 2012;94:1485-91. [PubMed]
- Dimitrova KR, Hoffman DM, Geller CM, et al. Radial artery grafting in women improves 15-year survival. J Thorac Cardiovasc Surg 2012. [Epub ahead of print]. [PubMed]
- Hayward PA, Buxton BF. Contemporary coronary graft patency: 5-year observational data from a randomized trial of conduits. Ann Thorac Surg 2007;84:795-9. [PubMed]
- Tatoulis J, Buxton BF, Fuller JA. Patencies of 2127 arterial to coronary conduits over 15 years. Ann Thorac Surg 2004;77:93-101. [PubMed]
- Collins P, Webb CM, Chong CF, et al. Radial artery versus saphenous vein patency randomized trial: five-year angiographic follow-up. Circulation 2008;117:2859-64. [PubMed]





