A meta-analysis of randomized controlled trials on mid-term angiographic outcomes for radial artery versus saphenous vein in coronary artery bypass graft surgery
Introduction
For selected patients with severe coronary artery disease, coronary artery bypass graft surgery (CABG) remains the superior management approach compared to percutaneous coronary interventions (1,2). The left internal mammary artery (LIMA) has long been established as the preferred conduit with the lowest long-term attrition rate, and is often selected for grafting the left anterior descending artery in conventional CABG (3,4). Conduit selection for the left circumflex and right coronary artery territories has been more variable amongst surgeons.
Currently, the saphenous vein (SV) and radial artery (RA) are the most commonly used conduits after LIMA for CABG. Although the use of RA was first reported in 1973 by Carpentier, it was not popularized until the 1990s, when antispasmodic medications and improved harvesting techniques were routinely used to prevent early spasm and occlusion (5). The use of SV was pioneered by Favaloro in the early years of CABG, but its early occlusion and long-term attrition rates have resulted in only half of all vein grafts being patent and without significant stenoses at 10-years (6,7). The aim of the present meta-analysis was to assess the existing evidence to compare mid-term angiographic outcomes of RA versus SV for CABG by using all available data from randomized controlled trials (RCTs).
Methods
Literature search strategy
Electronic searches were performed on Ovid Medline, Cochrane Central Register of Controlled Trials (CCTR), Cochrane Database of Systematic Reviews (CDSR), ACP Journal Club and Database of Abstracts of Review of Effectiveness (DARE) from their dates of inception to March 2013. To assess the highest level of available evidence according to the Centre for Evidence Based Medicine (CEBM) guidelines, only RCTs were included in the present meta-analysis (8). The search strategy included a combination of ‘radial artery’ and ‘randomized controlled trial’ as either keywords or MeSH headings. The reference lists of all retrieved articles were reviewed for further identification of potentially relevant studies. All relevant articles identified were assessed with application of the predefined selection criteria.
Selection criteria
Selected RCTs for the present meta-analysis included those that provided data on comparative angiographic outcomes for RA and SV after CABG. When institutions have published duplicate trials, only the most updated reports were included for qualitative appraisal. Measured ‘mid-term’ outcomes were limited to studies with follow-up beyond 3 years, consistent with previous reports (9). It is acknowledged that patient and coronary territory selection for revascularization varied amongst institutions and sometimes within an institution at different periods. All publications were limited to human subjects and English language. Abstracts, case reports, conference presentations, editorials and expert opinions were excluded.
Data extraction and critical appraisal
Data were extracted from texts, tables and figures of selected RCTs. When insufficient or ambiguous data were presented from publications, corresponding authors were contacted to provide additional information. Two investigators (S.A. and K.W.) independently reviewed each retrieved article. Discrepancies between the two reviewers were resolved by discussion and consensus with the senior investigators (C.C. and T.D.Y.).
Statistical analysis
Meta-analysis was performed by combining the reported angiographic incidences of complete occlusion, ‘string sign’, graft failure and complete patency. The odds ratio (OR) was used as a summary statistic. χ2 tests were used to study heterogeneity between trials. The I2 index was used to estimate the percentage of total variation across studies, due to heterogeneity rather than chance. An I2 value of greater than 50% was considered as substantial heterogeneity. If there was substantial heterogeneity, the possible clinical and methodological reasons for this were explored qualitatively. All P values were two-sided. All statistical analyses were conducted with Review Manager Version 5.1.2 (Cochrane Collaboration, Software Update, Oxford, UK).
Results
Quantity and quality of trials
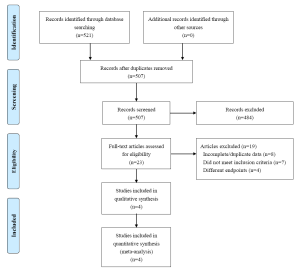
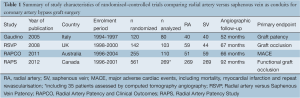
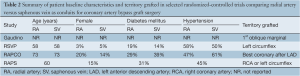
A total of 521 references were identified through the five electronic database searches. After exclusion of duplicate references, 507 potentially relevant articles were retrieved. After detailed evaluation of these articles, 23 studies remained for assessment. After applying the selection criteria, four RCTs were selected for quantitative assessment and meta-analysis (10-13). The search strategy is summarized in Figure 1, and the study characteristics of the selected RCTs are summarized in Table 1. Overall, 1,078 patients underwent randomization prior to CABG, with 831 mid-term angiographic results to compare RA (n=419) versus SV (n=412) grafts. Patient baseline characteristics and the grafted coronary territories are summarized in Table 2.
Full table
Full table
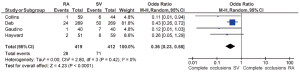
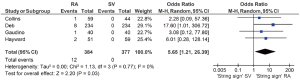
Assessment of complete occlusion
The incidence of complete occlusion was significantly lower after using RA compared to SV [6.7% vs. 17.2%; OR, 0.36; 95% confidence interval (CI), 0.23-0.58; P<0.0001; I2=0%], as summarized in Figure 2. The definition of ‘complete occlusion’ was consistent amongst trials.
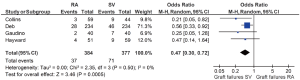
Assessment of ‘string sign’
The angiographic ‘string sign’ was significantly more likely to be identified after using RA compared to SV (3.1% vs. 0%; OR, 5.65; 95% CI, 1.21-26.39; P=0.03; I2=0%), as summarized in Figure 3. The definition of the ‘string sign’ was not elaborated in detail but generally considered as ‘severe diffuse graft narrowing’ (11,14).
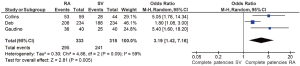
Assessment of graft failure
Graft failure was significantly lower after RA compared to SV (9.6% vs. 18.8%; OR, 0.47; 95% CI, 0.30-0.72; P=0.0005; I2=0%), as summarized in Figure 4. The definition of graft failure included complete occlusion and ‘string sign,’ as well as patients who had compromised flow state of >50% (11), stenosis of >80% (12) and Thrombolysis In Myocardial Infarction (TIMI) flow of 1-2 (13).
Assessment of complete patency
Complete graft patency, as defined by TIMI flow 3 (13) or ‘perfect patency’ (10,11), was found to be significantly higher after RA compared to SV (88.6% vs. 75.8%; OR, 3.19; 95% CI, 1.42-7.16; P=0.005; I2=59%), as summarized in Figure 5. Complete patency was not reported in one trial (12).
Discussion
Selection of the appropriate conduit for patients undergoing CABG is of paramount importance to minimize mortality and recurrence of symptoms. Additionally, the reduced need for repeat intervention remains a major advantage of CABG compared to PCI, especially for patients with severe coronary artery disease (2). The use of bilateral internal mammary arteries (BIMA) has been shown to confer a survival advantage for patients undergoing CABG (15,16). However, utilization of BIMA remains limited to a relatively low proportion of patients in the current clinical setting. The selection of SV or RA remains the most popular conduit choice for conventional CABG in combination with LIMA. However, observational data on mid-term clinical outcomes are conflicting, and the superiority of arterial conduits is not unanimously accepted by the cardiothoracic community (17).
The present systematic review identified four RCTs that presented data on angiographic outcomes of RA versus SV at follow-up beyond three years. Results of our meta-analysis demonstrated significantly higher incidences of graft failure and complete occlusion for SV, and significantly higher incidences of complete patency and the ‘string sign’ for RA at the time of the latest follow-up. These findings are consistent with large retrospective series, including a recent single-institutional study involving 1,851 patients that demonstrated significantly lower incidences of graft failure and higher incidences of patency for RA compared to SV (18). Similarly, a meta-analysis by Athanasiou and colleagues found that the RA was more likely to be patent at mid-term (1-5 years) (9). The superiority of RA angiographic outcomes may be partly explained by the differing pathophysiological process of venous and arterial atherosclerosis, with venous grafts being more likely to progress to concentric and diffuse lesions, that are vulnerable to rupture as a result of a less developed fibrous cap (19).
A number of limitations to our study should be acknowledged and interpretation of our results should not be generalized to all patients who undergo CABG. Firstly, it should be noted that patient selection and grafted territories differed between trials. However, all studies required eligible patients to demonstrate a minimum 70% proximal stenosis in their native coronary artery prior to randomization. This was partly because patients with less severe coronary artery disease are known to be more likely to suffer from graft failure and the effects of competitive flow, which has a more pronounced effect on arterial conduits (14,20). Secondly, it should be emphasized that angiographic endpoints and measurement systems differed between trials, with the primary endpoints ranging from graft patency (10), graft occlusion (11) and major adverse cardiac events (12). The Radial Artery Patency Study (RAPS) changed their primary endpoint from complete graft occlusion at 1-year (14) to functional graft occlusion beyond five years (13). Although the majority of data were derived from conventional angiograms, computed tomography angiograms were also employed in recent years to evaluate graft failures in this trial (13). These differences and the limited number of studies that presented data on complete patency may have contributed to the significant heterogeneity identified between trials. In addition, recent studies have suggested that specific subgroups such as male patients (21), elderly patients (22) and patients with diabetes mellitus (23) may derive more benefit from RA. It should be recognized that these potential prognostic factors differed significantly between trials, as summarized in Table 2, and may have influenced angiographic outcomes.
Ultimately, a multitude of factors relating to the conduit and the target coronary artery contribute to determining its long-term graft patency, including the selection of artery versus vein, harvesting technique, storage solution, as well as the size, severity of stenosis, and distal runoff of the native coronary artery (24). Using the available data from RCTs in the current literature, our meta-analysis suggests that radial arteries may be associated with superior angiographic outcomes compared to SV grafts for selected patients undergoing isolated CABG at mid-term follow-up. Future studies should correlate with clinical outcomes such as major adverse cardiac and cerebrovascular events and angina symptoms. Long-term follow-up data from the Veterans Affairs study may provide further robust data to compare RA and SV conduits (25). Novel surgical techniques such as endoscopic harvesting of conduits should also be examined.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Mohr FW, Morice MC, Kappetein AP, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet 2013;381:629-38. [PubMed]
- Cao C, Manganas C, Bannon P, et al. Drug-eluting stents versus coronary artery bypass graft surgery in left main coronary artery disease: a meta-analysis of early outcomes from randomized and nonrandomized studies. J Thorac Cardiovasc Surg 2013;145:738-47. [PubMed]
- Zeff RH, Kongtahworn C, Iannone LA, et al. Internal mammary artery versus saphenous vein graft to the left anterior descending coronary artery: prospective randomized study with 10-year follow-up. Ann Thorac Surg 1988;45:533-6. [PubMed]
- Acinapura AJ, Jacobowitz IJ, Kramer MD, et al. Internal mammary artery bypass: thirteen years of experience. Influence of angina and survival in 5125 patients. J Cardiovasc Surg (Torino) 1992;33:554-9. [PubMed]
- Carpentier A, Guermonprez JL, Deloche A, et al. The aorta-to-coronary radial artery bypass graft. A technique avoiding pathological changes in grafts. Ann Thorac Surg 1973;16:111-21. [PubMed]
- Favaloro RG, Effler DB, Cheanvechai C, et al. Acute coronary insufficiency (impending myocardial infarction and myocardial infarction): surgical treatment by the saphenous vein graft technique. Am J Cardiol 1971;28:598-607. [PubMed]
- Motwani JG, Topol EJ. Aortocoronary saphenous vein graft disease: pathogenesis, predisposition, and prevention. Circulation 1998;97:916-31. [PubMed]
- Centre for Evidence Based Medicine-Levels Of Evidence (March 2009). Oxford University. Accessed February 26, 2012.
- Athanasiou T, Saso S, Rao C, et al. Radial artery versus saphenous vein conduits for coronary artery bypass surgery: forty years of competition--which conduit offers better patency? A systematic review and meta-analysis. Eur J Cardiothorac Surg 2011;40:208-20. [PubMed]
- Gaudino M, Cellini C, Pragliola C, et al. Arterial versus venous bypass grafts in patients with in-stent restenosis. Circulation 2005;112:I265-9. [PubMed]
- Collins P, Webb CM, Chong CF, et al. Radial artery versus saphenous vein patency randomized trial: five-year angiographic follow-up. Circulation 2008;117:2859-64. [PubMed]
- Hayward PA, Buxton BF. The Radial Artery Patency and Clinical Outcomes trial: design, intermediate term results and future direction. Heart Lung Circ 2011;20:187-92. [PubMed]
- Deb S, Cohen EA, Singh SK, et al. Radial artery and saphenous vein patency more than 5 years after coronary artery bypass surgery: results from RAPS (Radial Artery Patency Study). J Am Coll Cardiol 2012;60:28-35. [PubMed]
- Desai ND, Cohen EA, Naylor CD, et al. A randomized comparison of radial-artery and saphenous-vein coronary bypass grafts. N Engl J Med 2004;351:2302-9. [PubMed]
- Kurlansky PA, Traad EA, Dorman MJ, et al. Thirty-year follow-up defines survival benefit for second internal mammary artery in propensity-matched groups. Ann Thorac Surg 2010;90:101-8. [PubMed]
- Lytle BW, Blackstone EH, Sabik JF, et al. The effect of bilateral internal thoracic artery grafting on survival during 20 postoperative years. Ann Thorac Surg 2004;78:2005-12; discussion 2012-4.
- Chung JW, Kim JB, Jung SH, et al. Mid-term outcomes of total arterial revascularization versus conventional coronary surgery in isolated three-vessel coronary disease. J Korean Med Sci 2012;27:1051-6. [PubMed]
- Tranbaugh RF, Dimitrova KR, Friedmann P, et al. Coronary artery bypass grafting using the radial artery: clinical outcomes, patency, and need for reintervention. Circulation 2012;126:S170-5. [PubMed]
- Hassantash SA, Bikdeli B, Kalantarian S, et al. Pathophysiology of aortocoronary saphenous vein bypass graft disease. Asian Cardiovasc Thorac Ann 2008;16:331-6. [PubMed]
- Botman CJ, Schonberger J, Koolen S, et al. Does stenosis severity of native vessels influence bypass graft patency? A prospective fractional flow reserve-guided study. Ann Thorac Surg 2007;83:2093-7. [PubMed]
- Schwann TA, Engoren M, Bonnell M, et al. Comparison of late coronary artery bypass graft survival effects of radial artery versus saphenous vein grafting in male and female patients. Ann Thorac Surg 2012;94:1485-91. [PubMed]
- Habib RH, Schwann TA, Engoren M. Late effects of radial artery versus saphenous vein grafting in patients aged 70 years or older. Ann Thorac Surg 2012;94:1478-84. [PubMed]
- Schwann TA, Al-Shaar L, Engoren M, et al. Late effects of radial artery vs. saphenous vein grafting for multivessel coronary bypass surgery in diabetics: a propensity-matched analysis. Eur J Cardiothorac Surg 2013. [Epub ahead of print]. [PubMed]
- Cao C, Manganas C, Byrom M, et al. Reply to the editor. J Thorac Cardiovasc Surg 2013;145:1147-8. [PubMed]
- Goldman S, Sethi GK, Holman W, et al. Radial artery grafts vs. saphenous vein grafts in coronary artery bypass surgery: a randomized trial. JAMA 2011;305:167-74. [PubMed]