Total arch replacement with separated graft technique and selective antegrade cerebral perfusion
Introduction
Surgical treatment of arch aneurysm or dissection has traditionally carried considerably high mortality and morbidity, particularly postoperative neurological dysfunction. The two major causes of postoperative neurological dysfunction are cerebral ischemic injury due to interruption of the cerebral circulation and cerebral embolism due to disloged atherosclerotic debris during the surgical procedure. Therefore, to improve surgical results it is crucial to protect the brain from ischemic and embolic injuries during the aortic arch repair. Three major techniques of cerebral protection have been used. These include: deep hypothermic circulatory arrest (DHCA) with or without retrograde cerebral perfusion (RCP) (1,2) and selective antegrade cerebral perfusion (SACP) (3). Whilst the methods used for brain protection are not standardized, and vary from institution to institution, there has been a recent trend towards increasing utilisation of SACP. In our institution, SACP with moderate hypothermia is the preferred method of cerebral protection during aortic arch replacement (4,5) because it supplies sufficient oxygenated blood to the brain, resulting in a more physiological brain energy metabolism (6).
Operative techniques
Preoperative setup
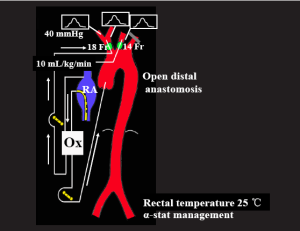
We routinely perform preoperative cerebral 4-vessel (bilateral internal carotid and vertebral arteries) angiography and cerebral computed tomographic scanning or magnetic resonance imaging to rule out cerebrovascular diseases, and to select the site of cerebral perfusion. Cardiopulmonary bypass (CPB) and SACP circuits are prepared and depicted in Figure 1. In addition to the major roller pump used for systemic perfusion, another roller pump for SACP is required. Real-time intraoperative monitoring of SACP is important to assess whether cerebral perfusion is adequate or not. We monitor cerebral perfusion pressure through the right radial arterial pressure and bilateral catheter tip pressure and perfusion flow rate. We also use two-channel serial EEG or BIS to monitor the electrical activity of brain, and two-channel near-infrared spectroscopy (NIRS) to estimate regional cerebral oxygenation. If available, we use internal jugular venous oxygen saturation to monitor cerebral oxygen saturation and transcranial Doppler sonography to measure the flow velocity in the middle cerebral artery.
Incision/exposure
The operation is performed through a median sternotomy with extensions of the incision to both supraclavicular regions. This approach allows us to reach the ascending aorta, aortic arch, arch vessels, and the descending thoracic aorta distal to the origin of the left subclavian artery. Even if the aneurysm is large in size, the descending aorta at the level of the tracheal bifurcation (T6) can usually be reached. However, if the aneurysm extends more distally, the following options are available: (I) use of the elephant trunk technique; (II) opening of the thoracic cavity by longitudinally incising the left pleura; (III) an additional left 4th intercostal space thoracotomy can be performed; or (IV) descending or thoracoabdominal replacement can be undertaken through the left thoracotomy.
Operation
Cardiopulmonary bypass
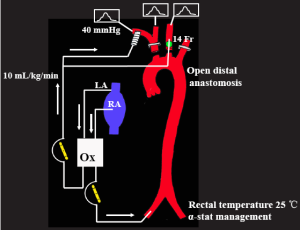
CPB is established by cannulating the ascending aorta, or the right axillary artery when necessary, with venous drainage obtained through a single two-staged cannula placed in the right atrium as shown in Figure 1. Before the ascending aorta is cannulated, epiaortic echo scanning and transesophageal echocardiography are routinely performed to assess whether atherosclerotic plaques are present in the ascending aorta and the aortic arch. The ascending aorta is cannulated using a Sarns Soft Flow aortic cannula (Terumo Cardiovascular Systems Corporation, Michigan USA), which provides excellent flow characteristics with less jetting. If the ascending aorta is found to be inappropriate for arterial cannulation by epiaortic echo scanning because of the presence of atherosclerotic debris, the preferred alternative site for arterial cannulation is the right axillary artery. If the right axillary artery is used, CPB and SACP circuits are modified as shown in Figure 2. After CPB is instituted, the left ventricular vent is inserted through the right superior pulmonary vein. Myocardial protection is provided by both antegrade and retrograde blood cardioplegia.
SACP protocol
When the patient is cooled down to a rectal temperature of 25 °C, systemic circulation is arrested, and the aorta is opened. Both innominate and the left common carotid arteries are completely transected 1 cm distal to the origin, where no atherosclerotic plaque or dissection is present, and the arteries are then cannulated through the transected vessel under direct vision. SACP is commenced at a rate of 10 mL/kg/min using a single roller pump, separate from the one used for systemic circulation. The left subclavian artery is kept cross-clamped during SACP except in the following cases where additional left subclavian artery perfusion is instituted: (I) occlusion of the right vertebral artery; (II) lack of adequate intracranial communication and (III) dominant left vertebral artery.
The radial artery pressure as well as bilateral catheter tip pressures are adjusted to maintain a mean perfusion pressure of around 40 mmHg. During CPB, arterial blood pH is managed utilizing alpha-stat strategy.
If the right axillary artery is selected for arterial perfusion, SACP technique is modified as follows (Figure 2): an 8 mm Dacron graft is sutured to the right axillary artery in an end-to-side fashion and systemic perfusion is carried out through both this graft and the femoral artery. After cooling to a rectal temperature of 25 °C, the origin of the innominate artery is cross-clamped. After systemic circulation is arrested, the left common carotid artery is cannulated and SACP flow (axillary and left common carotid artery flow) is maintained at 10 mL/kg/min.
More recently, unilateral cerebral perfusion through the right axillary artery instead of bilateral cerebral perfusion is used in selected patients undergoing hemiarch replacement for acute type A dissection. CPB is instituted through the right axillary artery and femoral artery. After cooling down to a rectal temperature of 25 °C, both innominate and left common carotid arteries are cross-clamped at their origins, and systemic circulatory arrest is induced. Subsequently unilateral cerebral perfusion through the right axillary artery is maintained at a flow rate of 10 mL/kg/min. This technique is used in selected patients requiring rather short duration of brain protection.
Operative technique of aortic arch repair
Two different kind of total arch replacement have been used in our series. One is the “island” or “en-bloc” technique in which arch vessels are re-implanted by suturing the aortic cuff containing the orifices of the arch vessels to the side hole of the arch graft, and the other is separated graft technique using four-branched aortic arch graft which is now our preferred technique. The separated branched graft technique has several advantages over the “island” technique including: (I) it can be safely used in the patient with degenerative, atherosclerotic aneurysm or acute type A aortic dissection and (II) vascular prostheses used for the separated graft technique are commercially available collagen-pretreated aortic arch graft with 4 branches (Hemashieled Branched Graft, Maquet) which helps to simplify the conduct of the operation.
Degenerative, atherosclerotic aneurysm of the aortic arch
Under SACP with systemic circulatory arrest, the distal end of the arch graft is sutured to the descending aortic stump. Antegrade perfusion is started from the side branch of the arch graft. The left subclavian artery is sutured to the third branch of the arch graft. Then re-warming by CPB is started. The proximal end of the arch graft is sutured to the ascending aortic stump. The coronary circulation is started after deairing the graft. The innominate and left common carotid arteries are then sutured to the corresponding branches of the arch graft. While performing the arch vessel anastomosis, the cannula is kept in place until two-third of the circumferential anastomosis is complete. Then the cannula is removed and blood perfusion through the cannula is discontinued.
Acute type A aortic dissection
We now use SACP through the right axillary artery and left common carotid artery as the preferred cerebral protection method. The surgical technique of the separated graft technique for acute type A dissection is essentially similar to that in atherosclerotic aneurysms except that obliteration of false lumen is performed, and the combined elephant trunk technique is adopted in case of dissection.
Postoperative care
Postoperative care in patients with aortic arch repair is essentially same as that in patients with other major cardiovascular operation.
Comments
On the basis of experimental and clinical studies, our current strategy for cerebral protection is that SACP is exclusively used for cases requiring longer cerebral protection time which exceeds 30 minutes (4,5).
SACP presents several advantages when compared to DHCA with or without RCP. They are: (I) SACP can extend the safe duration of cerebral protection up to 90 minutes, and facilitates complex aortic arch repair; (II) it obviates the need of deep hypothermia, thus reducing the pump time and the risk of hypothermia-related complications such as pulmonary insufficiency and coagulopathy; (III) SACP is more effective in supplying oxygenated blood to the brain, resulting in more physiological brain energy metabolism, and thus is the most reliable method of brain protection.
The suggested drawback of SACP includes the risk of cerebral embolism or malperfusion while cannulating the arch vessels. In order to avoid cerebral embolization of the dislodged atherosclerotic debris during arch vessel cannulation, special care should be taken as follows: (I) the arch vessels are transected about 1 cm distal to their origin where they are free from atherosclerotic debris, and then are cannulated through the transected vessel under direct vision; (II) in order to avoid cerebral malperfusion in acute aortic dissection, the true lumen can be distinguished from the false lumen when viewed from the aortic arch.
We have used two different kind of operative technique of arch repair as mentioned previously. Separated graft technique presents several advantages over the “en-bloc” or “island” technique (7). They include: (I) arch vessel anastomoses are performed at the intact distal arteries where they are free from atherosclerotic debris or dissection; (II) Pathological portions of the aortic arch can be completely resected in a Marfan’s patient; (III) bleeding from the site of the arch vessel anastomosis can be easily controlled; (IV) antegrade systemic perfusion through the arch graft prevents the retrograde embolization or organ malperfusion; and (V) total pump time and SACP time are shorter than those in the en-bloc technique.
Since we have adopted SACP and the separated graft technique in patients with acute type A dissection, we have become more aggressive at performing extended aortic arch replacement in selected patients (8,9). Our current indication for total arch replacement in these patients are: (I) acute aortic arch dissection with a tear in the aortic arch; (II) acute type A aortic dissection with a tear in the proximal descending aorta (retrograde type A dissection); (III) rupture or massive false lumen of the aortic arch; (IV) compromise of arch vessels; (V) coexistent aortic arch aneurysm; and (VI) young Marfan patient without serious dissection-related complications.
Permanent neurological dysfunction usually results from cerebral emboli and seems to have nothing to do with the cerebral protection method, although suboptimal protection will obviously aggravate any focal injury. Therefore, it is also critical to avoid embolic events during the operation through a number of important steps: (I) epiaortic echo scanning is routinely performed to select the site of ascending aortic cannulation; (II) the right axillary artery is used as an alternative site of cannulation if the ascending aorta is not suitable; (III) the arch vessels are transected where they are free from atherosclerosis and are cannulated under direct vision through the transected vessel; (IV) antegrade systemic perfusion through the side branch of the arch graft is commenced after the distal anastomosis is completed to prevent retrograde embolization; (V) the ascending or descending aorta containing clot or atheroma is completely resected and is replaced with the branched arch graft.
Over 500 patients have undergone surgery for aneurysm or dissection using moderate hypothermic SACP until the end of 2008. For the last 10 years 314 patients underwent aortic arch repair for aortic aneurysm or aortic dissection. Emergency operation was performed in 25% of the patients for rupture or acute aortic dissection. Total arch replacement was performed in 84% of the patients. In-hospital mortality was 3.8% and permanent neurological dysfunction and temporary dysfunction were 3.8% and 3.5%, respectively. Mean SACP time was 86 minutes in this series. There was no significant correlation between SACP time and in-hospital mortality or neurological dysfunction. Actuarial survival at 5-year is 76.4% and freedom from reoperation on the distal aorta is 85.3%.
Acknowledgements
The author thanks Dr Sean Galvin for his professional English narration.
Disclosure: The author declares no conflict of interest.
References
- Ergin MA, Galla JD, Lansman SL, et al. Hypothermic circulatory arrest in operations on the thoracic aorta. Determinants of operative mortality and neurologic outcome. J Thorac Cardiovasc Surg 1994;107:788-97; discussion 797-9. [PubMed]
- Ueda Y, Miki S, Kusuhara K, et al. Surgical treatment of aneurysm and dissection involving the ascending aorta and aortic arch utilizing circulatory arrest and retrograde cerebral perfusion. J Cardiovasc Surg (Torino) 1990;31:553-8. [PubMed]
- Bachet J, Guilmet D, Goudot B, et al. Antegrade cerebral perfusion with cold blood: a 13-year experience. Ann Thorac Surg 1999;67:1874-8; discussion 1891-4.
- Kazui T, Washiyama N, Muhammad BA, et al. Total arch replacement using aortic arch branched graftz with thee aid of antegrade selective cerebral perfusion. Ann Thorac Surg 2000;70:3-8; discussion 8-9. [PubMed]
- Kazui T, Washiyama N, Muhammad BA, et al. Improved results of atherosclerotic arch aneurysm with a refined technique. J Thorac Cardiovasc Surg 2001;121:491-9. [PubMed]
- Sakurada T, Kazui T, Tanaka H, et al. Comparative experimental study of cerebral protection during aortic arch reconstruction. Ann Thorac Surg 1996;61:1348-54. [PubMed]
- Di Eusanio M, Schepens MA, Morshuis WJ, et al. Separate grafts or en bloc anastomosis for arch vessels reimplantation to the aortic arch. Ann Thorac Surg 2004;77:2021-8. [PubMed]
- Kazui T, Kimura N, Yamada O, et al. Total arch graft replacement in patients with acute type A aortic dissection. Ann Thorac Surg 1994;58:1462-8. [PubMed]
- Kazui T, Washiyama N, Muhammad BA, et al. Extended total arch replacement for acute type A aortic dissection: experience with seventy patients. J Thorac Cardiovasc Surg 2000;119:558-65. [PubMed]





