The chimney-graft technique for preserving supra-aortic branches: a review
Introduction
Open surgical repair of pathologies of the aortic arch or the proximal descending aorta is associated with considerable periprocedural risks (1). Evolution in the endovascular era has influenced the management of aortic arch pathologies. Hybrid approaches for these patients have been proposed as alternative options (2,3). Despite the fact that following a hybrid strategy the need for sternotomy and cardiopulmonary by-pass is eliminated, the mortality and morbidity rates still remain relatively high (2). In addition, total endovascular techniques (i.e., fenestrated, branched devices) have been developed. However they need to overcome several anatomic and logistic limitations.
The chimney-graft technique, which was first described by Greenberg and associates (4) and was applied over the last decade for visceral debranching (5), could be a reasonable alternative for preserving supra-aortic branches in patients with pathologies involving the aortic arch.
We reviewed the published literature on the “chimney” or “snorkel” graft technique for the preservation of supra-aortic branches in order to provide an extensive insight of its feasibility and efficacy and investigate its outcomes.
Material and methods
Definition
The “chimney technique” involves deployment of stents/stent-grafts into the supra-aortic branches, with the proximal parts placed parallel to the main thoracic aortic endoprosthesis (between the aortic stent and the aortic wall) and extended above it to ensure perfusion.
Search strategy - eligibility criteria
Multiple electronic health database searches were performed that included Medline, Embase, Ovid, the Cochrane Database of Systematic Reviews, and the Cochrane Database of Abstracts of Reviews of Effectiveness (DARE), aiming to identify studies on “chimney technique” for the treatment of aortic arch pathologies. The search strategy was unrestricted and used exploded MeSH (medical subject heading) terms ‘double-barrel’, ‘triple-barrel’, ‘thoracoabdominal’, ‘aortic aneurysm’, ‘endovascular’, ‘chimney graft’, and/or ‘endovascular aortic arch debranching’. In addition, the references of all included articles were examined for further relevant series. All studies were independently assessed, and the full texts of the studies were retrieved.
Studies were included in the present review if (I) supra-aortic branches [left subclavian (LSA), left common carotid (LCCA) and innominate arteries (IA)] revascularization during endovascular treatment of aortic pathologies was achieved via a chimney graft (CG) implantation; and (II) the basic outcome criteria (complications rate; chimney graft patency, endoprosthesis related complications, and primary technical success rate; and the total mortality rate) were stated. Cases of prior thoracic endovascular aortic repair (TEVAR) failure treated with chimney grafts are also included in the present study. Reports on hybrid procedures and branched or fenestration stent-grafts were excluded as well as those detailing the chimney technique for visceral revascularization alone. Articles in languages other than English were also eliminated from further analysis. In cases of duplicated or metachronous publications from the same center, only the latest was included. Furthermore, several studies included patients with chimney graft implantation among other populations; they were included in the present review if separate data for this patient subgroup were provided.
All selected full-text articles were independently evaluated by two authors (S.M. and I.D.). From the attained articles the baseline patient data (mean age); indication of chimney technique application (aortic pathology or endoprosthesis-related complications after prior TEVAR); applied main aortic stent-graft design; number of chimney grafts and adjacent by-pass procedures were extracted and analyzed. Finally, the postoperative outcomes (primary technical success; mean follow-up period (months); endoprosthesis-related complications; post-procedural complications; and 30 d-/in-hospital mortality) were evaluated.
Results
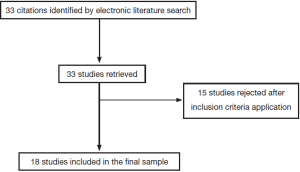
The electronic literature search yielded 18 reports that fulfilled the inclusion criteria (6-23) (Figure 1, Table 1). A total of 124 patients (79% male; mean age: range, 36-81.5) were analyzed. The aortic pathology was described in 108 patients: 28 (26%) had a degenerative aneurysm, 61 (56.5%) had aortic dissection, and 19 (17.5%) had other pathologies (type I endoleak, traumatic transection, penetrating ulcer, pseudoaneurysm).
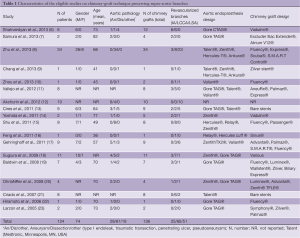
Full table
Various aortic endoprosthesis (Zenith®, Gore®, Talent®, etc.) were used for the thoracic aorta and numerous variable bare-stents or covered stents were selected for chimney-grafts. A total of 136 chimney grafts were implanted: 25 to the IA, 60 to the LCCA and 51 to the LSA. In 104 patients a single chimney graft was implanted whereas in 10 patients two chimney grafts were implanted.
It is noteworthy that there was a remarkable heterogeneity among studies regarding the revascularization of the left subclavian artery; some patients were treated with transposition of the LSA to the carotid artery, or carotid-subclavian bypass, or even no surgical revascularization. However, all patients underwent a carotid-to-carotid bypass before the aortic stent-graft was placed in zone 0 and the chimney-graft in the IA. Thus, a total of 28 adjacent by-pass procedures were performed.
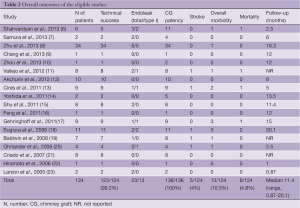
Technical success, endoleak rate, and CG patency
Primary technical success, defined as a complete chimney procedure, was achieved in 123/124 patients (99.2%). In the other patient, an infolding Viabahn® of the LCCA at the end of the procedure was detected, making it impossible to reline with another stent and thus an RCCA-LCCA bypass was performed. The overall endoleak rate was 18.5%; 13 patients (10.5%) developed a type I endoleak and 10 (8%) patients a type II endoleak. The majority of type I endoleaks resolved spontaneously or by coil embolization. In 5 patients with a type I endoleak angioplasty was performed, with another patient undergoing deployment of an additional aortic stent graft proximally in the ascending aorta to eliminate the endoleak. During a median follow-up period of 11.4 months (range, 0.87-20.1 months) all implanted chimney grafts remained patent.
Morbidity and mortality
Postoperatively 5 (4%) patients suffered a stroke. In addition, two patients developed paraplegia, one patient developed myocardial infarction, and another iliac hemorrhage. Therefore, the overall perioperative morbidity rate was 10.5%. Six patients (4.8%) died perioperatively: 1 died of lung cancer unrelated to chimney graft procedure and 2 died of stroke related to chimney graft deployment, whereas three more patients died due to undefined specific causes (Table 2).
Full table
Discussion
Treatment of aortic arch pathologies represents one of the greatest challenges in cardiothoracic surgery. So far there are four options:
Our study aimed to review the results of the chimney-graft technique for the treatment of aortic arch pathologies or extensive aortic lesions in which the aortic arch is involved. The analysis included a total of 124 patients in whom 136 chimney grafts were deployed. Interestingly, the technical success rate was 99.2%, demonstrating the feasibility of the procedure, and a chimney graft patency of 100%, at median follow-up of 11.4 months, illustrating the midterm safety of aortic arch vessels perfusion. The perioperative mortality rate was 4.8%, the stroke rate was 4% while events of spinal cord ischemia were rare. This can be justified first by the fact that, in the chimney technique, there is no need for aortic cross-clamping which eliminates the spinal cord ischemia time, and second by the fact that, for arch aneurysms, the length of aortic coverage with the endograft is relatively short. In 23 cases an endoleak (13 cases of Type Ia) was observed. Recent data suggest that temporarily maintaining elective aneurysmal sac perfusion may reduce the risk of neurologic events after endovascular repair of thoracoabdominal aneurysms and this point could also justify the rare incidence of paraplegia (24).
Sizing is crucial in achieving technical success. An ideal radial force should be exerted from the aortic endograft so as not to compromise the CG while maintaining adequate wall apposition. In the “chimney” technique, excess oversizing is needed to facilitate the formation of channels lateral to the graft in order to accommodate the chimney grafts (5,25). Chimney grafts, however, induce large “gutters” along the main endograft which may cause a proximal type I endoleak, representing the Achilles heel of the technique (5,26). The risk of endoleaks increase with the number of CGs implanted. In a recent review of 93 patients with juxtarenal or complex abdominal aortic aneurysms, the type I endoleak rate was 7.0% among patients who received one CG and 15.6% among patients with two CGs (5). In the present analysis the majority of the patients (104/124) received a single chimney graft whereas only 10 patients had two chimney grafts implanted; as such no further analysis regarding the risk of endoleak could be conducted.
While many techniques of open aortic arch reconstruction have evolved during the last three decades aimed at protecting the brain, stroke still remains a major complication of the procedure. Some of the techniques aim to suppress the metabolic demands of the brain while others aim to maintain the metabolic supply during systemic circulatory arrest. Currently, there are three basic strategies for an open arch reconstruction (1), including deep hypothermic circulatory arrest, hypothermia combined with retrograde cerebral perfusion, and moderate hypothermia with selective antegrade cerebral perfusion as proposed by Kazui (27). All three strategies have shown significant reduction of stroke when performed in centers of excellence and by experienced aortic surgeons. However, the technique that seems to demonstrate experimental and clinical superiority is selective antegrade cerebral perfusion (28).
Lately, several studies have described the use of a combined endovascular and open surgical approach for the treatment of arch pathologies. Hybrid repair of aortic arch pathologies has been considered a less invasive method; as a result, it presents an appealing option for high-risk patients who are unable to withstand an open repair. These “hybrid techniques” involve aortic arch debranching, thereby creating a proximal landing zone of adequate length, followed by stenting over the aortic arch (2,29,30). In a recent meta-analysis evaluating the hybrid repair of aortic arch pathologies the 30-day mortality rate for the “debranching” procedures was 11.9%, with a stroke rate of 7.6% and spinal cord ischemia rate of 3.6%. Cardiac complications occurred in 6.0% and renal insufficiency requiring permanent hemodialysis occurred in 5.7% of patients. The authors concluded that hybrid arch techniques provide a safe alternative to open repair with acceptable short- and mid-term results, although the stroke and mortality rates remain noteworthy (2).
Branched and fenestrated stent-grafts have been developed to treat aortic arch disease (3,31,32). In situ fenestration of aortic stent grafts is an alternative that eliminates the need for preoperative custom tailoring and offers a bailout option (33). However, these techniques require extensive manipulation in the aortic arch, which may cause high rates of adverse neurological events. Short- and mid-term data regarding the use of precurved fenestrated endografts appear encouraging. The results of a recent study evaluating fenestrated endograft treatment for thoracic aortic aneurysms and aortic dissection extended to the aortic arch showed that these devices are both safe and effective in carefully selected patients (3,31). In this study, 383 patients were treated with a precurved fenestrated endograft. The endografts were fabricated according to preoperative 3-dimensional computed tomographic images. The technical success rate was 95.8%. The 30-day mortality was 1.6%, while cerebrovascular accident occurred in 1.8% and permanent paralysis in 0.8%. Factors such as the inherent delay in device manufacturing, the high degree of planning and the cost are considerable limitations for the wider applications of the technique.
The outcome of open surgical reconstruction of the aortic arch is very inconsistent in the literature even when considering reports from centers of excellence. The stroke rate ranges from 2% to 13% and the peri-operative mortality ranges from 6.2% to 22% (34,35). The same inconsistency is noticed in the outcome of hybrid procedures as well. Stroke rates range from 0% to as high as 13% and the mortality rates range from 0 to 16% (36,37). Heterogeneous results also appeared in our analysis reporting total endovascular aortic arch exclusion with the use of chimneys. This is expected as the technique is newer and the case series have limited number of patients. Stroke rates ranged from 0 to 25.0% and mortality rates ranged from 0 to 18.2%.
The heterogeneity of the studies mentioned above makes the comparison of the various techniques difficult. In most studies the patients were not treated for the same disease. Some of them had aneurysmal degeneration of the aorta, while others had dissection or other pathologies. This mirrors the heterogeneity of the treated patients in terms of age and related comorbidities as well. Moreover, many centers that utilized hybrid or total endovascular techniques selected patients who were unfit or poor candidates for surgery. All these selection biases make comparison hazardous.
Conclusions
The “chimney” technique is a method that requires advanced endovascular skills. Endovascular aortic arch repair with chimney grafts is associated with a lower mortality rate compared to totally open and hybrid reconstruction. However, the stroke rate remains noteworthy. The technique has acceptable short term results. As there are no available longterm data, it should be approached with a skeptical view and a reasonable hesitation for a wide embracement of the method. Compared to fenestrated it has the advantage of avoiding the delay in device manufacturing and the high cost. Long-term data and larger series are needed to determine the safety and efficacy of this technique.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Coselli JS, Green SY. Evolution of aortic arch repair. Tex Heart Inst J 2009;36:435-7. [PubMed]
- Moulakakis KG, Mylonas SN, Avgerinos ED, et al. Hybrid open endovascular technique for aortic thoracoabdominal pathologies. Circulation 2011;124:2670-80. [PubMed]
- Azuma T, Yokoi Y, Yamazaki K. The next generation of fenestrated endografts: results of a clinical trial to support an expanded indication for aortic arch aneurysm treatment. Eur J Cardiothorac Surg 2013. [Epub ahead of print]. [PubMed]
- Greenberg RK, Clair D, Srivastava S, et al. Should patients with challenging anatomy be offered endovascular aneurysm repair? J Vasc Surg 2003;38:990-6. [PubMed]
- Moulakakis KG, Mylonas SN, Avgerinos E, et al. The chimney graft technique for preserving visceral vessels during endovascular treatment of aortic pathologies. J Vasc Surg 2012;55:1497-503. [PubMed]
- Shahverdyan R, Gawenda M, Brunkwall J. Triple-barrel graft as a novel strategy to preserve supra-aortic branches in arch-TEVAR procedures: clinical study and systematic review. Eur J Vasc Endovasc Surg 2013;45:28-35. [PubMed]
- Samura M, Zempo N, Ikeda Y, et al. Endovascular repair of distal arch aneurysm with double-chimney technique. Ann Thorac Surg 2013;95:1778-80. [PubMed]
- Zhu Y, Guo W, Liu X, et al. The Single-centre experience of the supra-arch chimney technique in endovascular repair of Type B aortic dissections. Eur J Vasc Endovasc Surg 2013;45:633-8. [PubMed]
- Chang G, Chen W, Yin H, et al. Endovascular repair of an aortic arch pseudoaneurysm by an atrial septal defect occluder combined with a chimney stent. J Vasc Surg 2013. [Epub ahead of print]. [PubMed]
- Zhou W, Zhou W, Qiu J. Endovascular repair of an aortic arch pseudoaneurysm with double chimney stent grafts: a case report. J Cardiothorac Surg 2013;8:80. [PubMed]
- Vallejo N, Rodriguez-Lopez JA, Heidari P, et al. Hybrid repair of thoracic aortic lesions for zone 0 and 1 in high-risk patients. J Vasc Surg 2012;55:318-25. [PubMed]
- Akchurin R, Imaev T, Komlev A, et al. TCT-123 Initial Experience of Chimney Technique in Case of Aortic Arch Pathologies Involving the Supra-Aortic Branches. J Am Coll Cardiol 2012;60: [PubMed]
- Cires G, Noll RE Jr, Albuquerque FC Jr, et al. Endovascular debranching of the aortic arch during thoracic endograft repair. J Vasc Surg 2011;53:1485-91. [PubMed]
- Yoshida RA, Kolvenbach R, Yoshida WB, et al. Total endovascular debranching of the aortic arch. Eur J Vasc Endovasc Surg 2011;42:627-30. [PubMed]
- Shu C, Luo MY, Li QM, et al. Early results of left carotid chimney technique in endovascular repair of acute non-a-non-B aortic dissections. J Endovasc Ther 2011;18:477-84. [PubMed]
- Feng R, Zhao Z, Bao J, et al. Double-chimney technology for treating secondary type I endoleak after endovascular repair for complicated thoracic aortic dissection. J Vasc Surg 2011;54:212-5. [PubMed]
- Gehringhoff B, Torsello G, Pitoulias GA, et al. Use of chimney grafts in aortic arch pathologies involving the supra-aortic branches. J Endovasc Ther 2011;18:650-5. [PubMed]
- Sugiura K, Sonesson B, Akesson M, et al. The applicability of chimney grafts in the aortic arch. J Cardiovasc Surg (Torino) 2009;50:475-81. [PubMed]
- Baldwin ZK, Chuter TA, Hiramoto JS, et al. Double-barrel technique for preservation of aortic arch branches during thoracic endovascular aortic repair. Ann Vasc Surg 2008;22:703-9. [PubMed]
- Ohrlander T, Sonesson B, Ivancev K, et al. The chimney graft: a technique for preserving or rescuing aortic branch vessels in stent-graft sealing zones. J Endovasc Ther 2008;15:427-32. [PubMed]
- Criado FJ. A percutaneous technique for preservation of arch branch patency during thoracic endovascular aortic repair (TEVAR): retrograde catheterization and stenting. J Endovasc Ther 2007;14:54-8. [PubMed]
- Hiramoto JS, Schneider DB, Reilly LM, et al. A double-barrel stent-graft for endovascular repair of the aortic arch. J Endovasc Ther 2006;13:72-6. [PubMed]
- Larzon T, Gruber G, Friberg O, et al. Experiences of intentional carotid stenting in endovascular repair of aortic arch aneurysms--two case reports. Eur J Vasc Endovasc Surg 2005;30:147-51. [PubMed]
- Harrison SC, Agu O, Harris PL, et al. Elective sac perfusion to reduce the risk of neurologic events following endovascular repair of thoracoabdominal aneurysms. J Vasc Surg 2012;55:1202-5. [PubMed]
- Lachat M, Frauenfelder T, Mayer D, et al. Complete endovascular renal and visceral artery revascularization and exclusion of a ruptured type IV thoracoabdominal aortic aneurysm. J Endovasc Ther 2010;17:216-20. [PubMed]
- Antoniou GA, Smyth JV, Antoniou SA, et al. Endoleak is the Achilles’ heel of the chimney technique for the treatment of complex aortic disease. Int Angiol 2012;31:595-6. [PubMed]
- Kazui T, Washiyama N, Muhammad BA, et al. Total arch replacement using aortic arch branched grafts with the aid of antegrade selective cerebral perfusion. Ann Thorac Surg 2000;70:3-8; discussion 8-9. [PubMed]
- Bachet J. What is the best method for brain protection in surgery of the aortic arch? Selective antegrade cerebral perfusion. Cardiol Clin 2010;28:389-401. [PubMed]
- Czerny M, Weigang E, Sodeck G, et al. Targeting landing zone 0 by total arch rerouting and TEVAR: midterm results of a transcontinental registry. Ann Thorac Surg 2012;94:84-9. [PubMed]
- Holt PJ, Johnson C, Hinchliffe RJ, et al. Outcomes of the endovascular management of aortic arch aneurysm: implications for management of the left subclavian artery. J Vasc Surg 2010;51:1329-38. [PubMed]
- Yokoi Y, Azuma T, Yamazaki K. Advantage of a precurved fenestrated endograft for aortic arch disease: simplified arch aneurysm treatment in Japan 2010 and 2011. J Thorac Cardiovasc Surg 2013;145:S103-9. [PubMed]
- Piffaretti G, Rivolta N, Fontana F, et al. Aortic arch aneurysm repair with a new branched device. J Vasc Surg 2013. [Epub ahead of print]. [PubMed]
- Riga CV, McWilliams RG, Cheshire NJ. In situ fenestrations for the aortic arch and visceral segment: advances and challenges. Perspect Vasc Surg Endovasc Ther 2011;23:161-5. [PubMed]
- Sundt TM 3rd, Orszulak TA, Cook DJ, et al. Improving results of open arch replacement. Ann Thorac Surg 2008;86:787-96; discussion 787-96. [PubMed]
- Jakob H, Tsagakis K, Tossios P, et al. Combining classic surgery with descending stent grafting for acute DeBakey type I dissection. Ann Thorac Surg 2008;86:95-101. [PubMed]
- Pochettino A, Brinkman WT, Moeller P, et al. Antegrade thoracic stent grafting during repair of acute DeBakey I dissection prevents development of thoracoabdominal aortic aneurysms. Ann Thorac Surg 2009;88:482-9; discussion 489-90. [PubMed]
- Melissano G, Bertoglio L, Civilini E, et al. Results of thoracic endovascular grafting in different aortic segments. J Endovasc Ther 2007;14:150-7. [PubMed]