Aortic arch surgery using moderate hypothermia and unilateral selective antegrade cerebral perfusion
Abstract
Background: Cerebral protection and circulatory management remains a controversial issue in aortic arch surgery. The present study reported surgical outcomes of arch repair using moderate hypothermic circulatory arrest (MHCA) and unilateral selective antegrade perfusion (uSACP).
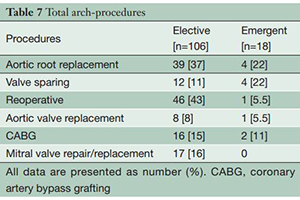
Methods: From January 2004 and December 2012, 500 patients underwent hemiarch repair (HARCH) and 124 underwent total arch replacement (TARCH) utilizing moderate hypothermic circulatory arrest with unilateral selective antegrade cerebral perfusion of the right axillary artery. Emergent surgery was required in 142 (28.4%) of HARCH patients and 18 (14.5%) of TARCH patients. Mean arrest temperature ranged from 25.6-27.2 ℃ for elective and emergent operations in both groups. Mean circulatory arrest was 26.8 minutes for hemiarch repairs and 54.2 minutes for total arch replacement.
Results: Overall mortality was 6.6% for hemiarch repairs and 9.7% for total arch replacements. Hospital mortality was 4.5% (16/358) and 10.4% (11/106) in elective cases, and 12% (17/142) and 5.6% (1/18) in elective cases, for hemiarch and total arch replacements respectively. Permanent neurological deficit (PND) occurred in 3 total arch replacement cases (2.4%). Multivariate analysis demonstrated that temperature was not found to be an independent risk factor during hemiarch or total arch replacements for mortality, permanent or neurological deficits, or renal failure.
Conclusions: Our approach for hemiarch and total arch repair utilizing MHCA and uSACP via the right axillary artery was associated excellent neurological and survival outcomes. Moderate hypothermia did not adversely impact cerebral or visceral organ protection.
Cover