A meta-analysis of deep hypothermic circulatory arrest alone versus with adjunctive selective antegrade cerebral perfusion
Introduction
Deep hypothermic circulatory arrest (DHCA) has been the cornerstone of aortic arch surgery since first popularized by Griepp et al. (Figure 1) (1). By reducing cerebral metabolic demands, brain protection can be achieved for durations sufficient to repair arch pathologies (2,3). While the extent of cerebral metabolic silencing is contingent on the arrest temperature, prolonged hypothermia has been adversely associated with coagulopathy and increased systemic inflammatory response (4,5).
By implementing selective antegrade cerebral perfusion (SACP) as an adjunct neuroprotection strategy, metabolic supply to the brain is maintained to better simulate normal physiologic conditions. As such, DHCA with SACP is reported to offer prolonged arrest durations (6), therefore allowing more complex arch operations to be performed.
However, significant concerns exist regarding the risks associated with SACP. These include the manipulation of epi-aortic vessels inadvertently causing atheromatous or air embolization and dissection of vessels, hypo- or hyper- cerebral perfusion leading to brain ischemia or oedema, reduced exposure of surgical field as impeded by cannulas, and technical complexities of axillary cannulation (7,8). The present meta-analysis aims to assess the clinical outcomes of SACP technique as an adjunct to DHCA.
Methods
Literature search strategy
Electronic searches were performed using Ovid Medline, PubMed, Cochrane Central Register of Controlled Trials (CCTR), Cochrane Database of Systematic Reviews (CDSR), ACP Journal Club, and Database of Abstracts of Review of Effectiveness (DARE) from their date of inception to January 2013. To achieve the maximum sensitivity of the search strategy and identify all studies, we combined the terms “cerebral perfusion” or “antegrade” and “circulatory arrest” and “aortic arch” as either key words or MeSH terms. The reference lists of all retrieved articles were reviewed for further identification of potentially relevant studies. All identified articles were systematically assessed using the inclusion and exclusion criteria. Expert academic cardiothoracic surgeons from the International Aortic Arch Surgery Study Group (IAASSG) formed the expert advisory panel and were asked whether they knew of any unpublished data.
Selection criteria
Eligible comparative studies for the present meta-analysis included those in which patient cohorts underwent DHCA alone, or DHCA with SACP, for aortic arch surgery. Circulatory arrest temperatures of comparative arms must be between 14.1 and 20 °C, determined either by protocol, or reported as minimal mean temperature. This temperature category was established by a recent Consensus of IAASSG (9), which classified profound (≤14 °C), deep (14.1-20 °C), moderate (20.1-28 °C) and mild (>28 °C) hypothermia utilized in arch surgery.
Studies that did not include stroke as a primary endpoint, or those whose primary patient set had a mean or median age less than 18 years old, were excluded. All publications were limited to those involving human subjects and in the English language. Abstracts, case reports, conference presentations, editorials, and expert opinions were excluded. Review articles were omitted because of potential publication bias and duplication of results. Studies that included fewer than 10 patients were also excluded.
Primary endpoints assessed included permanent neurological deficit (PND) and temporary neurological deficit (TND). Secondary endpoints included perioperative death, renal failure and reoperation for bleeding. PND was defined as stroke and/or coma and somnolence, while TND was defined as postoperative confusion, obtundation, agitation, delirium, focal deficits resolving within 24-72 hours, seizures or psychosis, or transient ischemic attacks. Perioperative death was defined as death occurring within 30 days or within the same hospital stay.
Data extraction and critical appraisal
All data were extracted from article texts, tables and figures. Two investigators (D.H.T. and B.W.) independently reviewed each retrieved article. Discrepancies between the two reviewers were resolved by discussion and consensus. The final results were confirmed by the senior investigator (T.D.Y.).
Statistical analysis
The odds ratio (OR) was used as a summary statistic. In the present study, both fixed- and random-effect models were tested. In a fixed-effects model, it was assumed that treatment effect in each study was the same, whereas in a random-effects model, it was assumed that there were variations between studies (10). χ2 tests were used to study heterogeneity between trials. I2 statistic was used to estimate the percentage of total variation across studies, owing to heterogeneity rather than chance, with values greater than 50% considered as substantial heterogeneity. Possible clinical and methodological reasons for any substantial heterogeneity were explored qualitatively where appropriate. In the present meta-analysis, the results using the random-effects model were presented to take into account the possible clinical diversity and methodological variation between studies. Specific analyses considering confounding factors were not possible due to absence of raw data.
Evidence of publication bias was sought using the methods of Egger et al. (11) and Begg et al. (10). Contour-enhanced funnel plot was performed to aid in interpretation of the funnel plot (12). If studies appear to be missing in areas of low statistical significance, then it is possible that the asymmetry is due to publication bias. If studies appear to be missing in areas of high statistical significance, then publication bias is a less likely cause of the funnel asymmetry. Intercept significance was determined by the t-test suggested by Egger et al. P<0.05 was considered representative of statistically significant publication bias.
All P values were 2-sided. All statistical analysis was conducted with Review Manager version 5.2.1 (Cochrane Collaboration, Software Update, Oxford, United Kingdom), or STATA version 11.0 (Stata Corporation, College Station, TX).
Results
Literature search
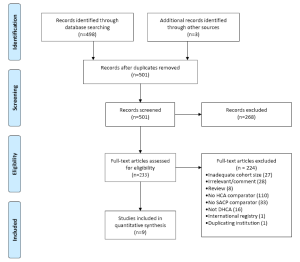
A total of 498 articles were identified through 6 electronic database searches. After exclusion of duplicate or irrelevant references, 233 potentially relevant studies were retrieved (Figure 2). Detailed evaluation of these texts yielded 9 studies that are included in the present meta-analysis (13-21), including one randomized trial (15). All remaining studies were observational studies.
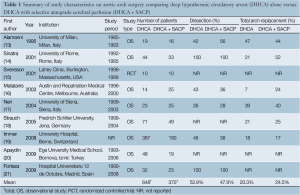
The study characteristics are summarised in Table 1. In total, 1,018 patients underwent aortic arch surgery, with 648 cases employing DHCA alone as neuroprotection strategy and 370 cases utilizing DHCA + SACP.
Full table
Demographic and operative characteristics
Similar comparative baseline characteristics were observed in both comparison arms. Males accounted for 65-86% of patients employing DHCA alone and 65-84% of those utilising DHCA + SACP, with no significant difference observed (mean: 72.0% vs. 70.8%; P=0.64). Average age ranged between 56-64.2 years and 58.4-66.5 years old (mean: 60.6 vs. 62.4; P=0.84). All other comparative preoperative characteristics were infrequently reported, including chronic pulmonary disease (16-18), hypertension (18,19), Marfan syndrome (16,17), and diabetes (17,18).
Frequency of dissection was similar in both cohorts. Apart from two studies specifically evaluating acute type A aortic dissections (14,21), dissection ranged from 26-73% and 28-56% for DHCA or DHCA + SACP (overall 52.8% vs. 47.9%; P=0.16) (13,16,17,19). The frequency of total arch replacement was also comparable in six studies that reported it; 20.3% of DHCA patients had total arch replacement, compared to 24.5% in the adjunct SACP group (P=0.26) (13,14,16-19).
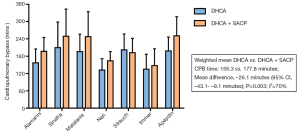
Cardiopulmonary bypass (CPB) time was significantly longer when neuroprotection was supplemented by SACP. With the exception of one study (18), all studies that reported CPB time demonstrated longer average CPB time (mean: 155.3 vs. 177.8 minutes; P=0.003; Figure 3) (13,14,16,17,19,20). Total cerebral protection time was also significantly longer for the DHCA + SACP group when reported in three studies (mean: 28.6 vs. 46.8 minutes; P=0.003) (17,18,20). No significant difference in circulatory arrest time was observed between the two cohorts (mean: 25.6 vs. 27.1 minutes; P=0.49) (13,14,16,18,19). A summary of neuroprotection strategies is presented in Table 2.

Full table
Primary endpoints - neurological outcomes
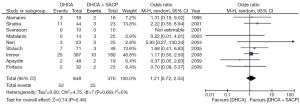
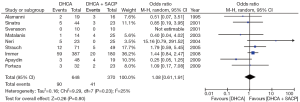
Permanent and temporary neurological deficits were reported in all studies. No significant difference was observed between DHCA and DHCA + SACP groups with respect to either PND [8.0% vs. 6.8%; OR, 1.21; 95% confidence interval (CI), 0.72-2.04; P=0.46; I2=0%; Figure 4] or TND (13.9% vs. 11.1%; OR, 1.08; 95% CI, 0.61-1.91; P=0.80; I2=25%; Figure 5). Subgroup analysis of unilateral (14,15,17,19-21), bilateral/island (13,16,18,19), or axillary/subclavian artery perfusion (15,17-19,21) demonstrated no significant difference in affecting PND or TND outcomes.
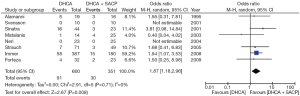
Secondary endpoint - mortality
Mortality outcomes were reported in all but one study (20). Overall, mortality was significantly lower when SACP was employed as a neuroprotection adjunct (DHCA vs. DHCA + SACP: 15.2% vs. 8.5%; OR, 1.87; 95% CI, 1.18-2.96; P=0.008; I2=0%; Figure 6).
Systemic outcomes
Four studies provided hospital outcomes, with comparable results between DHCA and DHCA with SACP (13.7 vs. 12.1 days; P=0.09; I2=74%) (16-19). Re-exploration for bleeding was reported in three studies, with comparable results (17.6% vs. 13.1%; P=0.42; I2=1%) (16-18). No other systemic outcomes were reported by more than two studies.
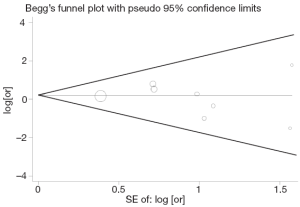
Publication bias
Begg’s funnel plot and Egger’s test were performed to assess publication bias in the literature. All 9 included studies yielded a Begg’s test score of P=0.711 and an Egger’s test score of P=0.684, while inspection of the contour-enhanced funnel plot (Figure 7) showed absence of publication bias in all 9 studies. These results suggest that publication bias was not an influencing factor.
Discussion
Effective neuroprotection during aortic arch surgery has significant bearing on patient outcomes. Early pioneers of arch surgery favoured hypothermic circulatory arrest (1) as hypothermia reduces cerebral metabolism sufficiently to allow for safe periods of circulatory arrest. This facilitates a bloodless operative field and more meticulous arch repair. Indeed, up to 30 minutes of safe arrest time can be tolerated when using DHCA alone (3,9). For more complex surgeries that require longer periods of circulatory arrest, the adjunctive supplementation of SACP fulfils any lingering cerebral metabolism that has not already been sufficiently moderated by DHCA, but concerns have been raised that SACP may introduce additional risks. Despite the cogency of these principles, no studies have thus far provided high-level clinical evidence to substantiate them. The present meta-analysis attempted to assess the effects of SACP in addition to DHCA.
Permanent neurological deficits following arch surgery is a significant and frequent contributor to postoperative outcomes. For example, in a large German retrospective registry of 1,558 patients with acute dissection, PND was reported in 13.4% of patients, with more than one-fifth of these patients dying within 30 days (22). PND has traditionally been recognized as embolic events, caused by inadvertent dislodgement of atheromatous plaques or introduction of gaseous emboli. The risk of these adverse events is anticipated to be higher during SACP due to manipulations of potentially plaque-laden epi-aortic vessels. Despite this, the present meta-analysis demonstrated the non-inferiority of using SACP. As this particular cohort had longer CPB time and more total arch replacements, which reflects potentially higher surgical risk profiles, SACP may even be beneficial when confounding factors are adjusted. These findings can partly be accounted for by the evolutionary improvements in surgical handling and deairing techniques, introduction of axillary artery cannulation, and optimisation of perfusate delivery. Furthermore, Hagl and associates hypothesized that clinically- and radiologically-silent embolic infarcts may only be detectable when exacerbated by mild diffuse cerebral injuries caused by failure to meet remaining cerebral metabolic demands (23). Fulfilment of lingering metabolism by SACP may also contribute to the comparable stroke rates, as sustained cerebral perfusion may mitigate the exacerbation of clinically-silent infarcts.
Subtle damages to the brain parenchyma is also of keen interest to surgeons, as TND significantly reduces short- and long-term quality of life (24,25). While DHCA at 20 °C only sufficiently reduces cerebral metabolic rates to 24% of baseline, SACP is able to maintain near physiological blood flow (3), and therefore should logically provide better protection against TND. However, in a randomized study of 20 arch surgery patients allocated to DHCA or DHCA with SACP, Svensson and colleagues determined that supplementary SACP did not offer better neuroprotection, with DHCA patients significantly outperforming SACP patients on a battery of neurocognitive tests (15). Furthermore, Gega and colleagues also report that for patients whose professions require higher cognition, such as doctors and lawyers, DHCA alone at 19 °C did not diminish their mental capacities (26). These results are in line with the findings of the present meta-analysis, which did not demonstrate advantage of adjunctive SACP in reducing TND.
Over the past three decades, survival from arch surgery has also improved steadily, with reductions in mortality rates to single-digits (6,26-28). However, despite the increasing application of SACP, several studies have indicated that the duration and use of SACP has no significant correlation to mortality (29,30), although this has been disputed by others (14,31). In a study of 220 patients undergoing SACP, Kazui et al. demonstrated that the majority of deaths were not related to cerebral events, but mostly due to organ failure and other perfusion-related issues (32). Multiple studies have further associated mortality with preoperative risk factors such as age, renal and liver dysfunction, and cardiogenic shock (5,21,33). In the present meta-analysis, SACP was preferentially utilized for more complex arch cases. Despite this, patients undergoing DHCA with SACP demonstrated significantly more favourable pooled mortality rate (15.2% vs. 8.5%; OR, 1.87; P=0.008). The reasons for this observation cannot be clearly explained by the present meta-analysis without ascertaining the original raw data, as there is a lack of detailed reporting in terms of the causes of perioperative mortality. Plausible explanations may include SACP improving cerebral protection and associated stroke-related death, and the more recent introduction of SACP producing temporal effects due to evolving improvements in surgical experience and techniques.
The present study is limited by several key constraints. Firstly, most studies reported in the literature are retrospective observational studies, except one small-scale RCT which was underpowered to detect any significant clinical difference. Significant confounding factors and intrinsic patient selection bias associated with these reports weakened the overall pooled effect of the meta-analysis. Therefore the present study should not be used to reach conclusive recommendations, but can only be used to generate hypotheses for future higher-level clinical trials. Important variables such as dissection pathology, extent of arch replacement, and heterogenous surgical techniques, have not been compensated for due to the lack of original patient data. Given the inconsistency in the reporting of clinical endpoints, it is difficult to perform cross comparisons on several important clinical endpoints. The literature is even more unclear in terms of the benefits of SCAP in relatively straightforward aortic arch cases, such as hemi-arch replacement and cases requiring 20-30 minutes of circulatory arrest, or in situations where SACP is only initiated partway through surgery when arrest time becomes unexpectedly lengthened.
A comprehensive multi-institutional registry focusing on surgical strategies and outcomes is therefore required to overcome the above limitations. More consistent reporting of outcomes and collaborative pooling of raw patient data to enable risk-stratification and propensity matching will serve as a better-powered platform in lieu of randomized controlled trials, and will also assist in patient selection and prognostication. Existing registries are limited to particular arch pathologies and do not examine surgical techniques in sufficient details (22,34), and are therefore unsuitable for this purpose. Multi-institutional arch database and prospective trials evaluating neuroprotection strategies, overseen by the IAASSG, have significant potential to overcome the limitations faced by existing observational reports.
In summary, our findings showed that SACP does not occasion higher incidence of PND or TND, and is associated with improved perioperative mortality outcome, although the reasons for this are unclear. The data suggested that implementation of SACP in addition to DHCA may be beneficial for longer durations of circulatory arrest. The added complexities of perfusate delivery and aortic vessel manipulations require institutions to be sufficiently experienced with this technique.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Griepp RB, Stinson EB, Hollingsworth JF, et al. Prosthetic replacement of the aortic arch. J Thorac Cardiovasc Surg 1975;70:1051-63. [PubMed]
- Stecker MM, Cheung AT, Pochettino A, et al. Deep hypothermic circulatory arrest: I. Effects of cooling on electroencephalogram and evoked potentials. Ann Thorac Surg 2001;71:14-21. [PubMed]
- McCullough JN, Zhang N, Reich DL, et al. Cerebral metabolic suppression during hypothermic circulatory arrest in humans. Ann Thorac Surg 1999;67:1895-9; discussion 1919-21.
- Kamiya H, Hagl C, Kropivnitskaya I, et al. The safety of moderate hypothermic lower body circulatory arrest with selective cerebral perfusion: a propensity score analysis. J Thorac Cardiovasc Surg 2007;133:501-9. [PubMed]
- Easo J, Weigang E, Hölzl PP, et al. Influence of operative strategy for the aortic arch in DeBakey type I aortic dissection - analysis of the German Registry for Acute Aortic Dissection Type A. Ann Cardiothorac Surg 2013;2:175-80.
- Di Eusanio M, Schepens MA, Morshuis WJ, et al. Antegrade selective cerebral perfusion during operations on the thoracic aorta: factors influencing survival and neurologic outcome in 413 patients. J Thorac Cardiovasc Surg 2002;124:1080-6. [PubMed]
- Matalanis G, Galvin S. “Branch-first” continuous perfusion aortic arch replacement and its role in intra-operative cerebral protection. Ann Cardiothorac Surg 2013;2:194-201.
- Griepp RB, Griepp EB. Perfusion and cannulation strategies for neurological protection in aortic arch surgery. Ann Cardiothorac Surg 2013;2:159-62.
- Yan TD, Bannon PG, Bavaria J, et al. Consensus on hypothermia in aortic arch surgery. Ann Cardiothorac Surg 2013;2:163-8.
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088-101. [PubMed]
- Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-34. [PubMed]
- Palmer TM, Peters JL, Sutton AJ, et al. Contour-enhanced funnel plots for meta-analysis. Stata Journal 2008;8:242-54.
- Alamanni F, Agrifoglio M, Pompilio G, et al. Aortic arch surgery: pros and cons of selective cerebral perfusion. A multivariable analysis for cerebral injury during hypothermic circulatory arrest. J Cardiovasc Surg (Torino) 1995;36:31-7. [PubMed]
- Sinatra R, Melina G, Pulitani I, et al. Emergency operation for acute type A aortic dissection: neurologic complications and early mortality. Ann Thorac Surg 2001;71:33-8. [PubMed]
- Svensson LG, Nadolny EM, Penney DL, et al. Prospective randomized neurocognitive and S-100 study of hypothermic circulatory arrest, retrograde brain perfusion, and antegrade brain perfusion for aortic arch operations. Ann Thorac Surg 2001;71:1905-12. [PubMed]
- Matalanis G, Hata M, Buxton BF. A retrospective comparative study of deep hypothermic circulatory arrest, retrograde, and antegrade cerebral perfusion in aortic arch surgery. Ann Thorac Cardiovasc Surg 2003;9:174-9. [PubMed]
- Neri E, Sassi C, Barabesi L, et al. Cerebral autoregulation after hypothermic circulatory arrest in operations on the aortic arch. Ann Thorac Surg 2004;77:72-9; discussion 79-80. [PubMed]
- Strauch JT, Böhme Y, Franke UF, et al. Selective cerebral perfusion via right axillary artery direct cannulation for aortic arch surgery. Thorac Cardiovasc Surg 2005;53:334-40. [PubMed]
- Immer FF, Moser B, Krähenbühl ES, et al. Arterial access through the right subclavian artery in surgery of the aortic arch improves neurologic outcome and mid-term quality of life. Ann Thorac Surg 2008;85:1614-8; discussion 1618. [PubMed]
- Apaydin AZ, Islamoglu F, Askar FZ, et al. Immediate clinical outcome after prolonged periods of brain protection: retrospective comparison of hypothermic circulatory arrest, retrograde, and antegrade perfusion. J Card Surg 2009;24:486-9. [PubMed]
- Forteza A, Martín C, Centeno J, et al. Acute type A aortic dissection: 18 years of experience in one center (Hospital 12 de Octubre). Interact Cardiovasc Thorac Surg 2009;9:426-30. [PubMed]
- Krüger T, Weigang E, Hoffmann I, et al. Cerebral protection during surgery for acute aortic dissection type A: results of the German Registry for Acute Aortic Dissection Type A (GERAADA). Circulation 2011;124:434-43. [PubMed]
- Hagl C, Ergin MA, Galla JD, et al. Neurologic outcome after ascending aorta-aortic arch operations: effect of brain protection technique in high-risk patients. J Thorac Cardiovasc Surg 2001;121:1107-21. [PubMed]
- Krähenbühl ES, Immer FF, Stalder M, et al. Temporary neurological dysfunction after surgery of the thoracic aorta: a predictor of poor outcome and impaired quality of life. Eur J Cardiothorac Surg 2008;33:1025-9. [PubMed]
- Ergin MA, Uysal S, Reich DL, et al. Temporary neurological dysfunction after deep hypothermic circulatory arrest: a clinical marker of long-term functional deficit. Ann Thorac Surg 1999;67:1887-90; discussion 1891-4.
- Gega A, Rizzo JA, Johnson MH, et al. Straight deep hypothermic arrest: experience in 394 patients supports its effectiveness as a sole means of brain preservation. Ann Thorac Surg 2007;84:759-66. [PubMed]
- Patel HJ, Nguyen C, Diener AC, et al. Open arch reconstruction in the endovascular era: analysis of 721 patients over 17 years. J Thorac Cardiovasc Surg 2011;141:1417-23. [PubMed]
- Leshnower BG, Myung RJ, Kilgo PD, et al. Moderate hypothermia and unilateral selective antegrade cerebral perfusion: a contemporary cerebral protection strategy for aortic arch surgery. Ann Thorac Surg 2010;90:547-54. [PubMed]
- Kazui T, Yamashita K, Washiyama N, et al. Usefulness of antegrade selective cerebral perfusion during aortic arch operations. Ann Thorac Surg 2002;74:S1806-9; discussion S1825-32.
- Di Bartolomeo R, Di Eusanio M, Pacini D, et al. Antegrade selective cerebral perfusion during surgery of the thoracic aorta: risk analysis. Eur J Cardiothorac Surg 2001;19:765-70. [PubMed]
- Khaladj N, Shrestha M, Meck S, et al. Hypothermic circulatory arrest with selective antegrade cerebral perfusion in ascending aortic and aortic arch surgery: a risk factor analysis for adverse outcome in 501 patients. J Thorac Cardiovasc Surg 2008;135:908-14. [PubMed]
- Kazui T, Washiyama N, Muhammad BA, et al. Total arch replacement using aortic arch branched grafts with the aid of antegrade selective cerebral perfusion. Ann Thorac Surg 2000;70:3-8; discussion 8-9. [PubMed]
- Iba Y, Minatoya K, Matsuda H, et al. Contemporary open aortic arch repair with selective cerebral perfusion in the era of endovascular aortic repair. J Thorac Cardiovasc Surg 2013;145:S72-7. [PubMed]
- Trimarchi S, Nienaber CA, Rampoldi V, et al. Contemporary results of surgery in acute type A aortic dissection: The International Registry of Acute Aortic Dissection experience. J Thorac Cardiovasc Surg 2005;129:112-22. [PubMed]





