Systematic review and meta-analysis of two decades of reported outcomes for robotic coronary artery bypass grafting
Introduction
In the last two and a half decades, robotic coronary artery bypass grafting (CABG) has emerged as the most minimally invasive method of coronary bypass surgery. Loulmet and colleagues in Paris first introduced this technique in 1998, and its practicality has grown with each new generation of robotic systems, aided by advancements in supporting technology like epicardial stabilizers and devices for distal anastomosis (1-3).
Robotic CABG encompasses robot-assisted minimally invasive direct coronary artery bypass (RA-MIDCAB) and totally endoscopic coronary artery bypass (TECAB). In RA-MIDCAB, robotic assistance is utilised in the harvest of the internal thoracic artery (ITA) whilst the anastomosis is performed under direct visualisation through an anterior mini-thoracotomy, and is typically performed on a beating heart, facilitated by endostabilizers. In TECAB, the entire operation is performed totally endoscopically and can be done either on-pump, off-pump or on-pump with a beating heart (4).
Robotic CABG has evolved from a method capable of single-vessel to complex multi-vessel revascularisation (5). Specialised centres that regularly perform TECAB have demonstrated its effectiveness in providing multivessel, multiarterial revascularisation, even for high-risk patients such as those who are diabetic, elderly, obese and undergoing repeat procedures (6). Nowadays, robotic CABG can also be applied alongside percutaneous coronary intervention (PCI) in a hybrid coronary revascularization (HCR) approach to treat multivessel disease (2,4).
Robotic assistance is associated with less perioperative morbidity and enhanced recovery stemming from reduced surgical trauma, shorter recovery time and earlier return to normal activities (4,5). The safety and efficacy of robotic CABG has been demonstrated consistently in the literature (7-9), with decreased conversion rates and improved outcomes with experience and careful patient selection (10). Previous meta-analysis and retrospective review of TECAB and RA-MIDCAB have concluded acceptable mortality risk and early graft patency, with outcomes comparable to a traditional sternotomy approach (1,10,11).
Nevertheless, the robotic approach faces significant challenges and requires extensive training, which explains its slow adoption with only few dedicated programs continuing its use (6). A successful robotic cardiac program requires significant infrastructure costs and training of a skilled multidisciplinary team. However, although the initial procedures required longer operative times, these durations have decreased significantly over the past two decades (11), and there is some evidence to suggest that its higher procedural costs may be counterbalanced by lower complication rates and shorter length of intensive care unit (ICU) and hospital stays, providing a potentially cost neutral alternative (12).
This article aims to provide a comprehensive review of the last two decades of literature on the status and outcomes of both RA-MIDCAB and TECAB by pooling the reported peri-operative and follow-up outcomes through a meta-analytic approach, with a focus on freedom from major adverse cardiac and cerebrovascular events (MACCE) and overall graft patency.
Methods
Literature search
This study has been conducted and reported in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) 2020 statement (13). Ethics approval was not required for this study given all data was retrieved from previously published studies. Three electronic databases, MEDLINE via PubMed, Embase and Cochrane Central Register of Controlled Trials (CENTRAL), were systematically searched from their date of inception to August 2023. Search terms included “coronary artery bypass” and “robot” or “robotic” or “robot assisted” or “RA-MIDCAB” or “TECAB” or “totally endoscopic” (Appendix 1). Reference lists from previous reviews, meta-analyses and included articles were also reviewed for further suitable studies.
Inclusion and exclusion criteria
Studies reporting outcomes on adult patients undergoing robotic CABG were included in this systematic review. For the meta-analysis, studies were grouped by the type of robot-assisted CABG procedure performed. The first group included patients who underwent RA-MIDCAB only, the second group included TECAB procedures only, and the third group included studies in which all robotic CABG procedures were combined into a single cohort. Included studies were limited to involving human subjects, had full text available, were not conference abstracts or case reports, and were written in the English language. To partially account for the impact of the learning curve, studies with ten or less patients in the cohort of successful robotic CABG were excluded. RA-MIDCAB studies were also excluded where the anastomosis was performed through a non-thoracotomy approach (i.e., through median sternotomy). Where multiple papers of overlapping cohorts were found, only the most updated, largest or cohort with the longest follow-up reported was included. In the case of multiple competing factors for inclusion, articles reporting graft patency rates were preferred.
Data collection and quality appraisal
Three authors (B.H., J.R., K.W.) independently performed the study selection, data extraction and quality appraisal using a pre-formed template. Data items pertaining to study characteristics, patient characteristics, operative details, peri-operative and follow-up outcomes were collected. The quality of each included study was assessed using the modified Canadian National Institute of Health Economics (CNIHE) quality appraisal checklist for case series (14). Studies were considered high quality if they scored sixteen or more points out of nineteen, moderate quality if scored twelve to fifteen, and low quality if eleven or less points were scored. Any discrepancies between the reviewers were resolved by means of discussion until consensus was reached.
Primary and secondary outcomes
The primary outcomes investigated were mid-to-long term graft patency, freedom from reintervention and from major adverse cardiac events (MACE) or MACCE. Secondary outcomes included overall survival in the follow-up period, as well as perioperative outcomes such as in-hospital mortality, rate of myocardial infarction (MI), stroke, reoperation for bleeding, new onset arrhythmia, pulmonary complication, acute renal injury, wound infection, ICU and hospital length of stays.
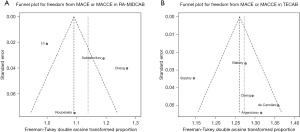
Statistical methods
Baseline patient characteristics and operative outcomes, where reported by half or more of included studies, were pooled using meta-analysis of proportions or means for categorical and continuous variables, respectively, using R (Version 4.1.2, R Foundation for Statistical Computing, Vienna, Austria). Where values were reported as a median and range, mean and standard deviation (SD) estimates were calculated using methods described by Wan and colleagues (15). A random effects model and the restricted maximum likelihood estimate method was used to derive the pooled weighted estimates. Pooled data was presented as n (%) with 95% confidence intervals (CIs). Heterogeneity was assessed using the I2 statistic with a value of 0–49%, 50–74% and ≥75% deemed as low, moderate and high heterogeneity, respectively. Publication bias was assessed through the small-study effect methods with a funnel plot. Tests for funnel plot asymmetry such as Egger’s regression test were only used when there were greater than ten studies to be sufficiently powered.
Results
Study selection
The electronic literature search yielded a total of 531 studies, of which 460 studies from database sources and six from citations underwent title and abstract screening following exclusion of duplicates. One hundred and four articles altogether underwent full-text review, of which 62 were excluded for reasons outlined in Figure 1. Of the remaining 39 studies included in the meta-analysis, seventeen studies reported outcomes on RA-MIDCAB only, ten studies reported on TECAB only, three studies provided separate data for both RA-MIDCAB and TECAB, and nine studies reported outcomes for a combined robotic CABG cohort. All included studies were retrospective observational cohorts (Table 1), the majority of which were single institutional studies, however nine (7,10,22,24,42,44-47) were multicenter or database analyses.

Table 1
| Primary author | Ref. | Year | Institution(s)/database | Study period | Follow-up (months) | Robotic CABG approach | No. of patients | CPB |
|---|---|---|---|---|---|---|---|---|
| Lo | (17) | 2023 | Taichung Veterans General Hospital, Taiwan | 2005–2015 | 77.0±44.9 | RA-MIDCAB | 562 | OPCAB |
| Jonsson | (18) | 2023 | Emory University School of Medicine, USA | 2009–2020 | 46±35.6 | RA-MIDCAB | 1,000 | OPCAB |
| Torregrossa | (19) | 2022 | Lankenau Heart Insititute, USA | 2005–2021 | 88.5±67.0 | RA-MIDCAB | 600 | OPCAB |
| Gofus | (12) | 2022 | University Hospital Hradec Kralove, Czechia | 2018–2021 | 18 | RA-MIDCAB | 130 | OPCAB |
| Piperata | (20) | 2022 | Hopital Cardiologique de Haut-Leveque, Bordeaux University Hospital, France | 2021–2022 | NA | RA-MIDCAB | 17 | ONCAB |
| Varrone | (21) | 2022 | Surgery, Lenox Hill Hospital, Northwell Health, New York, NY, USA | 1997–2021 | NA | RA-MIDCAB | 1,080 | OPCAB |
| Cheng | (3) | 2021 | PLA General Hospital, China | 2007–2017 | 89.7±30.4 | RA-MIDCAB; TECAB | 154; 126 | OPCAB |
| Patrick | (22) | 2021 | STS Adult Cardiac Surgery Database (98 institutions) | 2014–2019 | NA | RA-MIDCAB | 1,195 | OPCAB [1,070], ONCAB [125] |
| Wu | (23) | 2019 | Kaohsiung Veterans General Hospital, Taiwan | 2010–2016 | 6 | RA-MIDCAB | 22 | OPCAB [12], ONCAB [10] |
| Giambruno | (10) | 2018 | Western University, London Health Sciences Centre (Canada), University of California Davis (USA), Saint Boniface Hospital (Canada) | 1998–2016 | NA | RA-MIDCAB | 605 | OPCAB [589], ONCAB [16] |
| Pasrija | (24) | 2018 | STS Adult Cardiac Surgery Database | 2011–2014 | NA | RA-MIDCAB; TECAB | 50; 50 | OPCAB |
| Roubelakis | (25) | 2017 | OLV Hospital, Belgium | 2002–2015 | 60.8±120.3 | RA-MIDCAB | 44 | OPCAB [43], ONCAB [1] |
| Sabashnikov | (26) | 2014 | Royal Brompton & Harefield NHS Foundation Trust, UK | 2003–2013 | 57±17.3 | RA-MIDCAB | 236 | OPCAB |
| Bayramoglu | (27) | 2014 | Florence Nightingale Hospital, Turkey | 2004–2012 | 60.3±23.8 | RA-MIDCAB | 100 | OPCAB |
| Fujita | (28) | 2014 | National Cerebral and Cardiovascular Center, Osaka, Japan | 2004–2012 | NA | RA-MIDCAB | 33 | OPCAB |
| Ishikawa | (29) | 2014 | Kanazawa University, Kanazawa, Japan | 2005–2013 | NA | RA-MIDCAB | 35 | OPCAB |
| Leyvi | (30) | 2014 | Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY, USA | 2007–2012 | NA | RA-MIDCAB | 150 | ONCAB [7], OPCAB [143] |
| Turner | (31) | 2006 | Center for Advanced Surgery and Technology, Trinity Mother Frances Health System and University of Texas at Tyler, College of Nursing and Health Science, Tyler, Texas | 2004–2005 | NA | RA-MIDCAB | 70 | OPCAB |
| Derose | (32) | 2005 | St. Luke’s-Roosevelt Hospital Center, USA | 2002–2004 | 16.1±8.4 | RA-MIDCAB | 37 | OPCAB |
| Falk | (33) | 2000 | University of Leipzig, Germany | 1998–1999 | 3 | RA-MIDCAB; TECAB | 32; 22 | OPCAB |
| Balkhy | (34) | 2022 | University of Chicago, USA | 2018–2020 | 1.4±1 | TECAB | 192 | OPCAB |
| Balkhy | (35) | 2020 | University of Chicago, USA | 2013–2018 | 22.5±15.1 | TECAB | 361 | OPCAB |
| Stastny | (36) | 2018 | Innsbruck Medical University, Austria | 2001–2012 | 82.8±27.6 | TECAB | 208 | ONCAB |
| Zaouter | (37) | 2015 | CHU de Bordeaux, Service d’Anesthésie-Réanimation II, Bordeaux, France | 2011–2014 | NA | TECAB | 38 | OPCAB |
| Dhawan | (38) | 2012 | University of Chicago, USA | 2007–2009 | NA | TECAB | 106 | OPCAB |
| Jegaden | (39) | 2011 | Hospital Louis Pradel, France | 2003–2008 | 32.4±1.2 | TECAB | 59 | OPCAB |
| Srivastava | (40) | 2010 | Alliance Hospital (Odessa Regional Medical Center), USA | 2004–2007 | 17.6±23.2 | TECAB | 241 | OPCAB |
| de Cannière | (7) | 2007 | Erasme University Hospital, Belgium; Klinikum der Johann Wolfgang Goethe Universität, Germany; Dresden Herzzentrum, Germany; Onze Lieve Vrouwziekenhuis, Belgium; Leipzig Heart Institute, Germany | 1998–2002 | 6 | TECAB | 228 | OPCAB [111], ONCAB [117] |
| Mishra | (41) | 2006 | Escorts Heart Institute and Research Centre, India | 2002–2005 | 1–24 | TECAB | 13 | OPCAB [11], ONCAB [2] |
| Argenziano | (42) | 2006 | Milstein Hospital, USA; Henrico Doctors’ Hospital, USA; Leopold-Franzen-Universitat Innsbruck, Austria; Alliance Hospital, USA; St Joseph Hospital of Atlanta, USA; Saint Agnes Medical Center, USA; Lenox Hill Hospital, USA; Sacred Heart Medical Center, USA; New York Presbyterian Hospital, USA | 2002–2004 | 3 | TECAB | 85 | ONCAB |
| Al-Mulla | (43) | 2022 | Heart Hospital, Hamad Medical Corporation, Qatar | 2009–2020 | 3 | Mixed | 71 | NA |
| Cerny | (44) | 2021 | OLV Hospital, Belgium; University Hospital Hradec Kralove, Czechia; University Hospital Bordeaux, France; Erasme University Hospital, Belgium | 2016–2019 | NA | Mixed | 1,266 | OPCAB [1,250], ONCAB [16] |
| Yokoyama | (45) | 2021 | National Inpatient Sample | 2012–2017 | NA | Mixed | 7,355 | NA |
| Whellan | (46) | 2016 | STS Adult Cardiac Surgery Database | 2006–2012 | NA | Mixed | 9,862 | OPCAB [7,655], ONCAB [2,207] |
| Cavallaro | (47) | 2015 | Nationwide Inpatient Sample | 2008–2010 | NA | Mixed | 2,582 | OPCAB [2,060] ONCAB [522] |
| Casula | (48) | 2014 | University Hospital of Central Manchester, UK | 2002–2008 | NA | Mixed | 100 | OPCAB |
| Currie | (49) | 2012 | London Health Sciences Centre, Canada | 1999–2003 | 96±16 | Mixed | 82 | OPCAB |
| Folliguet | (50) | 2010 | L’Institut Mutualiste Montsouris, France | 2004–2008 | 13±36 | Mixed | 56 | OPCAB |
| Mishra | (51) | 2007 | Escorts Heart Institute and Research Centre, India | 2002–2006 | 1–42 | Mixed | 268 | NA |
CABG, coronary artery bypass grafting; CPB, cardiopulmonary bypass; OPCAB, off-pump coronary artery bypass grafting; ONCAB, on-pump coronary artery bypass grafting; NA, not applicable; TECAB, totally endoscopic coronary artery bypass.
Quality appraisal
Of the 39 studies evaluated using the CNIHE quality appraisal checklist, seven studies overall were considered high quality, 25 studies were moderate quality and seven were low quality (Appendix 2). The majority of studies deemed low quality were as a result of inadequate length of follow-up.
Baseline patient characteristics
From 1998 to 2022, the reported outcomes of 6,152 patients who underwent RA-MIDCAB, 1,729 patients who underwent TECAB and 21,642 patients who underwent either form of robotic CABG were analysed separately. The pooled weighted estimates for patient and operative characteristics in each group are displayed in Tables 2-4.
Table 2
| Characteristics | Pooled weighted estimate (95% CI)* | I2 % statistic (No. of studies reported) |
|---|---|---|
| Baseline patient characteristics | ||
| Age (years) | 64.5 (61.9–67.2) | 99% (20/20) |
| Male gender (%) | 75.8 (73.0–78.4) | 79% (20/20) |
| BMI (kg/m2) | 27.5 (26.6–28.3) | 99% (12/20) |
| Single vessel disease (%) | 75.5 (49.5–89.7) | 99% (13/20) |
| Double vessel disease (%) | 18.9 (7.8–39.2) | 99% (10/20) |
| Triple vessel disease (%) | 17.0 (5.9–39.9) | 99% (9/20) |
| LAD lesion (%) | 91.2 (61.9–98.5) | 100% (10/20) |
| Smoker (%) | 44.7 (37.4–52.3) | 94% (13/20) |
| Diabetes mellitus (%) | 39.4 (30.8–48.7) | 98% (17/20) |
| Hypertension (%) | 78.5 (71.0–84.5) | 95% (14/20) |
| Chronic lung disease (%) | 11.2 (7.3–16.6) | 94% (11/20) |
| Chronic kidney disease (%) | 5.7 (2.3–13.5) | 97% (12/20) |
| Prior MI (%) | 26.9 (17.7–38.5) | 98% (13/20) |
| Prior PCI (%) | 37.2 (28.4–46.9) | 97% (11/20) |
| LVEF (%) | 57.0 (53.2–60.7) | 98% (12/20) |
| HCR (%) | 31.1 (24.2–38.9) | 92% (9/20) |
| Operative characteristics | ||
| Operative time (min) | 273.4 (125.6–421.3) | 100% (10/20) |
| Off-pump | 5,976/6,152 (97.1%) | – |
| LIMA-LAD anastomosis (%) | 98.3 (96.2–99.2) | 81% (13/20) |
| Conversion to sternotomy (%) | 2.7 (1.5–4.8) | 85% (14/20) |
| Blood transfusion (%) | 8.4 (6.0–11.5) | 71% (9/20) |
*, data are presented as pooled weighted estimate (95% CI) with the exception of n/N (%) for “Off-pump”. RA-MIDCAB, robot-assisted minimally invasive direct coronary artery bypass; CI, confidence interval; BMI, body mass index; LAD, left anterior descending; MI, myocardial infarction; PCI, percutaneous coronary intervention; LVEF, left ventricular ejection fraction; HCR, hybrid coronary revascularisation; LIMA, left internal mammary artery.
Table 3
| Characteristics | Pooled weighted estimate (95% CI)* | I2 % statistic (No. of studies reported) |
|---|---|---|
| Baseline patient characteristics | ||
| Age (years) | 61.9 (59.8–64.1) | 94% (13/13) |
| Male gender (%) | 76.8 (69.7–82.6) | 87% (12/13) |
| BMI (kg/m2) | 28.2 (25.8–30.6) | 97% (6/13) |
| Single vessel disease (%) | 86.1 (61.9–96.0) | 98% (9/13) |
| Double vessel disease (%) | 11.1 (2.2–40.0) | 98% (7/13) |
| Triple vessel disease (%) | 4.2 (2.3–7.5) | 46% (6/13) |
| LAD lesion (%) | 95.7 (87.7–98.6) | 93% (9/13) |
| Smoker (%) | 4.0 (2.5–4.0) | 86% (8/13) |
| Diabetes mellitus (%) | 3.2 (2.5–4.0) | 87% (10/13) |
| Hypertension (%) | 75.8 (66.2–83.4) | 92% (10/13) |
| Chronic kidney disease (%) | 3.6 (1.3–10.0) | 92% (6/13) |
| Prior MI (%) | 25.1 (20.3–30.7) | 66% (8/13) |
| Prior PCI (%) | 29.7 (14.9–50.6) | 95% (5/13) |
| LVEF (%) | 56.9 (53.8–60.0) | 96% (11/13) |
| HCR (%) | 29.2 (21.6–38.1) | 91% (8/13) |
| Operative characteristics | ||
| Operative time (min) | 272.9 (226.0–319.9) | 99% (10/13) |
| Off-pump | 1,638/1,729 (94.7%) | – |
| LIMA-LAD anastomosis (%) | 95.2 (89.9–97.8) | 88% (11/13) |
| Conversion to sternotomy (%) | 2.9 (1.1–7.3) | 91% (12/13) |
| Conversion to RA-MIDCAB (%) | 4.7 (1.1–18.2) | 93% (6/13) |
| Blood transfusion (%) | 17.4 (8.1–33.6) | 95% (6/13) |
*, data are presented as pooled weighted estimate (95% CI) with the exception of n/N (%) for “Off-pump”. TECAB, totally endoscopic coronary artery bypass; CI, confidence interval; BMI, body mass index; LAD, left anterior descending; MI, myocardial infarction; PCI, percutaneous coronary intervention; LVEF, left ventricular ejection fraction; HCR, hybrid coronary revascularisation; LIMA, left internal mammary artery; RA-MIDCAB, robot-assisted minimally invasive direct coronary artery bypass.
Table 4
| Characteristics | Pooled weighted estimate (95% CI)* | I2 % statistic (No. of studies reported) |
|---|---|---|
| Baseline patient characteristics | ||
| Age (years) | 62.2 (58.8–65.7) | 99% (8/9) |
| Male gender (%) | 83.0 (75.9–88.3) | 99% (9/9) |
| Single vessel disease (%) | 77.8 (42.0–94.4) | 99% (4/9) |
| Double vessel disease (%) | 15.9 (5.4–38.6) | 98% (4/9) |
| Triple vessel disease (%) | 11.8 (5.9–22.0) | 85% (4/9) |
| Diabetes mellitus (%) | 3.1 (2.2–4.0) | 99% (8/9) |
| Hypertension (%) | 69.9 (49.5–84.6) | 100% (5/9) |
| Chronic lung disease (%) | 14.1 (9.5–21.0) | 99% (5/9) |
| Chronic kidney disease (%) | 6.5 (2.4–16.7) | 100% (4/9) |
| Prior MI (%) | 22.9 (11.4–40.7) | 100% (6/9) |
| HCR (%) | 11.4 (6.8–18.8) | 84% (5/9) |
| Operative characteristics | ||
| Operative time (min) | 249.8 (117.6–381.9) | 99% (4/9) |
| Off-pump | 11,215/13,962 (80.3%) | – |
| Conversion to sternotomy (%) | 3.3 (2.1–5.2) | 34% (5/9) |
| Blood transfusion (%) | 12.4 (9.1–16.7) | 93% (4/9) |
*, data are presented as pooled weighted estimate (95% CI) with the exception of n/N (%) for “Off-pump”. CABG, coronary artery bypass grafting; CI, confidence interval; MI, myocardial infarction; HCR, hybrid coronary revascularisation.
Baseline patient demographics in terms of mean age, proportion of male patients, body mass index (BMI) and comorbidities including hypertension, diabetes, smoking history, chronic lung disease, chronic kidney disease and prior MI were similar amongst patients receiving either RA-MIDCAB or TECAB. The majority of patients were 60–65 years of age, three quarters were male, and on average were overweight, but not obese. A quarter of patients had an MI previously, with 29.7% (95% CI: 14.9–50.6%; I2=95%) in the TECAB group and 37.2% (95% CI: 28.4–46.9%, I2=97%) in the RA-MIDCAB group having undergone previous PCI. Approximately a third of patients in both groups were planned as part of an HCR approach, which more commonly occurred after the robotic CABG procedure. A greater proportion of TECAB recipients were observed to have single vessel disease (86.1%; 95% CI: 61.9–96.0%, I2=98%) whereas more patients in the RA-MIDCAB group had triple vessel disease (17.0%; 95% CI: 5.9–39.9%, I2=99%), which reflects the preference for RA-MIDCAB in multivessel disease. Mean left ventricular ejection fraction (LVEF) was normal and the same amongst TECAB and RA-MIDCAB recipients at approximately 57%.
Operative characteristics
In all included articles except one (26), the da Vinci Robotic System (Intuitive Surgical, Sunnyvale, CA, USA) was used. Most procedures were performed on a beating heart (97.1% in RA-MIDCAB and 94.7% in TECAB). The mean operative time was similar for both RA-MIDCAB and TECAB at approximately 273 minutes. In the vast majority of cases, a left internal mammary artery to left anterior descending (LIMA-LAD) anastomosis was performed. Rate of conversion to sternotomy across RA-MIDCAB and TECAB was 2.7% (95% CI: 1.5–4.8%; I2=85%) and 2.9% (95% CI: 1.1–7.3%; I2=91%), respectively. In the TECAB group, conversion to RA-MIDCAB occurred at a rate of 4.7% (95% CI: 1.1–18.2%; I2=93%) in reported studies. Number of patients requiring a blood transfusion peri-operatively was higher for patients receiving TECAB at 17.4% (95% CI: 8.1–33.6%; I2=95%) compared to 8.4% (95% CI: 6.0–11.5%; I2=71%) receiving RA-MIDCAB.
Perioperative outcomes
In-hospital mortality was 0.9% (95% CI: 0.6–1.4%; I2=38%) for RA-MIDCAB recipients in 18 studies, and 1.5% (95% CI: 0.9–2.4%; I2=8%) for TECAB recipients in 12 studies (Tables 5,6). In the mixed robotic CABG group comprising largely of data from national databases, the pooled in-hospital mortality was 0.9% (95% CI: 0.7–1.3%; I2=66%). On average, perioperative stroke occurred in less than 1% of patients, perioperative MI in less than 2%. Other perioperative complications such as acute renal injury, new onset atrial fibrillation, wound infection, pulmonary complications, re-operation for bleeding and requirement for prolonged ventilation greater than 24 hours was observed at a higher rate in the TECAB group (Table 6). However, length of ICU and hospital stay was observed to be longer in the RA-MIDCAB group at 40.8 hours (95% CI: 25.3–56.3; I2=99%) and 7.6 days (95% CI: 5.2–10.0; I2=100%), respectively, compared to 32.8 hours (95% CI: 24.3–41.3; I2=76%) and 6.0 days (95% CI: 3.8–8.3; I2=99%), respectively, in the TECAB group.
Table 5
| Outcome | Pooled weighted estimate (95% CI) | I2 % statistic (No. of studies reported) |
|---|---|---|
| Perioperative outcome | ||
| Early mortality (%) | 0.9 (0.6–1.4) | 38% (18/20) |
| Perioperative stroke (%) | 0.9 (0.6–1.3) | 17% (14/20) |
| Perioperative MI (%) | 1.3 (0.9–1.8) | 0% (13/20) |
| Re-operation for bleeding (%) | 1.9 (1.5–2.5) | 13% (12/20) |
| Arrhythmia (%) | 7.9 (3.6–16.2) | 97% (10/20) |
| Pulmonary complication (%) | 2.5 (1.1–5.6) | 73% (8/20) |
| Acute renal injury (%) | 1.2 (0.7–2.3) | 72% (13/20) |
| Wound infection (%) | 1.3 (0.6–2.7) | 67% (13/20) |
| ICU length of stay (hours) | 40.8 (25.3–56.3) | 99% (11/20) |
| Hospital length of stay (days) | 7.6 (5.2–10.0) | 100% (15/20) |
| Mid-to-long term outcomes | ||
| Mean follow-up time (months) | 62.6 (38.0–87.3) | – (7/11) |
| Completeness of follow-up (%) | 96.2 (85.5–99.1) | – (8/11) |
| All-cause mortality (%) | 9.3 (2.3–31.3) | 99% (8/11) |
| Cardiac mortality (%) | 2.7 (0.6–10.5) | 73% (4/11) |
| Freedom from MACE or MACCE (%) | 83.2 (72.0–90.5) | 90% (4/11) |
| Reintervention (%) | 5.5 (2.6–11.3) | 93% (7/11) |
| Overall graft patency (%) | 96.2 (93.8–98.2) | 0% (5/11) |
| Stroke (%) | 2.0 (1.5–2.8) | 0% (6/11) |
| MI (%) | 2.7 (1.5–4.7) | 64% (7/11) |
RA-MIDCAB, robot-assisted minimally invasive direct coronary artery bypass; CI, confidence interval; MI, myocardial infarction; ICU, intensive care unit; MACE, major adverse cardiac events; MACCE, major adverse cardiac and cerebrovascular events.
Table 6
| Outcome | Pooled weighted estimate (95% CI) | I2 % statistic (No. of studies reported) |
|---|---|---|
| Perioperative outcome | ||
| Early mortality (%) | 1.5 (0.9–2.4) | 8% (12/13) |
| Perioperative stroke (%) | 0.9 (0.5–1.8) | 0% (8/13) |
| Perioperative MI (%) | 1.6 (0.9–2.9) | 0% (7/13) |
| Re-operation for bleeding (%) | 3.1 (1.6–6.0) | 73% (10/13) |
| Arrhythmia (%) | 10.6 (7.9–14.0) | 42% (7/13) |
| Pulmonary complication (%) | 3.6 (2.3–5.5) | 10% (6/13) |
| Acute renal injury (%) | 3.1 (1.5–6.2) | 51% (5/13) |
| Wound infection (%) | 1.8 (0.4–6.9) | 50% (5/13) |
| ICU length of stay (hours) | 32.8 (24.3–41.3) | 76% (9/13) |
| Hospital length of stay (days) | 6.0 (3.8–8.3) | 99% (10/13) |
| Mid-to-long term outcomes | ||
| Mean follow-up time (months) | 48.9 (6.1–91.8) | – (5/9) |
| Completeness of follow-up (%) | 94.1 (85.1–97.8) | – (4/9) |
| All-cause mortality (%) | 3.4 (1.1–9.9) | 42% (4/9) |
| Freedom from MACE or MACCE (%) | 91.7 (86.7–94.9) | 76% (5/9) |
| Reintervention (%) | 4.1 (2.2–7.5) | 63% (6/9) |
| Overall graft patency (%) | 96.4 (93.0–98.9) | 71% (9/9) |
| Recurrent angina (%) | 3.5 (0.7–15.3) | 77% (4/9) |
TECAB, totally endoscopic coronary artery bypass; CI, confidence interval; MI, myocardial infarction; ICU, intensive care unit; MACE, major adverse cardiac events; MACCE, major adverse cardiac and cerebrovascular events.
Mid-to-long term outcomes
Eleven studies in the RA-MIDCAB group reported mid-to-long term follow-up data (Table 5). The mean follow-up time was 62.6 months in the RA-MIDCAB group with 96.2% completeness of follow-up. Overall all-cause mortality in this follow-up period was 9.3% (95% CI: 2.3–31.3%; I2=99%), however cardiac cause of mortality was 2.7% (95% CI: 0.6–10.5%; I2=73%). Freedom from MACE or MACCE was 83.2% (95% CI: 72.0–90.5%; I2=90%), with a post-operative stroke and MI rate of 2.0% (95% CI: 1.5–2.8%; I2=0%) and 2.7% (95% CI: 1.5–4.7%; I2=64%), respectively, in the follow-up period. The overall graft patency rate, as assessed in a total of 403 patients with either computed tomography (CT) or angiography, was 96.2% (95% CI: 93.8–98.2%; I2=0%), and the rate of coronary re-intervention was 5.5% (95% CI: 2.6–11.3%; I2=93%).
In the nine studies reporting on mid-to-long term outcomes of TECAB, the mean follow-up time was 48.9 months with 94.1% completeness of follow-up (Table 6). All-cause mortality was 3.4% (95% CI: 1.1–9.9%; I2=42%) and freedom from MACE or MACCE was 91.7% (95% CI: 86.7–94.9%; I2=76%). Recurrent angina was experienced in 3.5% of patients and rate of postoperative MI was 1.3%. Overall graft patency, as assessed in 900 patients, and reintervention rate were similar to the RA-MIDCAB group.
Five studies with a mixed robotic CABG cohort reported on mid-to-long term outcomes with a mean follow-up time of 54.5 months and a 95.1% completeness of follow-up (Table 7). Overall all-cause mortality was 1.3% (95% CI: 0.04–26.4%; I2=80%) with freedom from MACE or MACCE of 88.8% (95% CI: 82.7–93%; I2=2%). The overall graft patency as assessed in 144 patients was 90.7% (95% CI: 84.6–94.5%; I2=0%) and coronary reintervention was required in 4.7% (95% CI: 2.5–8.5%; I2=0%) of recorded patients.
Table 7
| Outcome | Pooled weighted estimate (95% CI) | I2 % statistic (No. of studies reported) |
|---|---|---|
| Perioperative outcome | ||
| Early mortality (%) | 0.9 (0.7–1.3) | 66% (8/9) |
| Perioperative stroke (%) | 0.7 (0.3–2.1) | 97% (5/9) |
| Re-operation for bleeding (%) | 3.2 (1.5–6.8) | 99% (8/9) |
| Acute renal injury (%) | 5.3 (2.4–11.3) | 99% (4/9) |
| Hospital length of stay (days) | 5.9 (4.0–7.8) | 100% (9/9) |
| Mid-to-long term outcomes | ||
| Mean follow-up time (months) | 54.5 (47.2–58.1) | – (2/5) |
| All-cause mortality (%) | 1.3 (0.04–26.4) | 80% (2/5) |
| Freedom from MACE or MACCE (%) | 88.8 (82.7–93) | 2% (2/5) |
| Reintervention (%) | 4.7 (2.5–8.5) | 0% (3/5) |
| Overall graft patency (%) | 90.7 (84.6–94.5) | 0% (3/5) |
CABG, coronary artery bypass grafting; CI, confidence interval; MACE, major adverse cardiac events; MACCE, major adverse cardiac and cerebrovascular events.
Publication bias
On visual inspection of funnel plots for primary outcomes, there was asymmetry in all funnel plots except for overall graft patency in the RA-MIDCAB group (Figures 2,3). There were insufficient studies for Egger’s regression test to be applied.

Discussion
In this current era, there exists a multitude of alternative, less invasive approaches to the “gold standard” on-pump sternotomy CABG, including off-pump, minimally invasive and totally endoscopic techniques. Despite these growing advances, there has been a slow uptake and plateau of robotic assistance for CABG, with many sites discontinuing the procedure for at least one year (46). A multitude of factors may be contributing to this, such as the perceived steep learning curve, albeit less so in those already adept with minimally invasive technology. Moreover, comparison of minimally invasive techniques with conventional CABG in the literature have often yielded equivalent results, hence surgeons may remain reluctant to adopt these more technically demanding approaches (30). The heterogeneity of the patient cohort seen in this meta-analysis may reflect that at current, no single cohort for whom robotic CABG is most suitable has been identified and this may also contribute to low adoption rates.
Despite this, there has been a growing number of participating centers since recent renewed interest owing to technological advancements, more structured training pathways and reconfirmation of superiority of CABG over PCI in various clinical scenarios (35,44). Advanced robotic systems now provide enhanced high-definition three-dimensional (3D) visualisation together with improved control, dexterity and precision from four robotic arms (12). Moreover, at two and a half decades since the first adoption of this technique, the long-term data that was previously lacking is now increasingly available and showing encouraging outcomes. In a propensity-matched analysis of robotic versus conventional CABG by Kofler and colleagues, there was no difference in perioperative outcomes, long-term survival or freedom from MACCE, with rates of MI (1.4%), stroke (0.7%), early mortality (1.3%) comparable to the current meta-analysis (52). In more recent and larger propensity-matched analysis of the US National Inpatient Sample from 2012 to 2017, robotic CABG was found to be associated with lower in-hospital mortality, rate of acute kidney injury, transfusion, post-operative bleeding and hospital length of stay compared to conventional CABG (45).
Although all-cause mortality in the follow-up period of this pooled meta-analysis is high, at 9.3% for RA-MIDCAB and 3.4% for TECAB, this is likely confounded by deaths unrelated to a primary coronary cause. Thus, freedom from MACCE and long-term graft patency may be more relevant indicators for long-term effectiveness and durability of revascularisation compared to overall survival. In this pooled meta-analysis, freedom from MACE or MACCE of 83.2% and 91.7% in RA-MIDCAB and TECAB, respectively, at a mean follow-up of 5.2 years appears greater than five-year MACCE-free survival of 81% of conventional CABG from the more recent NOBLE randomised trial (53).
Graft patency is also an important indicator of the durability of robotic CABG. In this pooled meta-analysis, the overall graft patency rate was excellent at 96% for both RA-MIDCAB and TECAB, as assessed through either invasive or CT angiography in a mean follow-up period up to five years. This is comparable to the ten-year patency rate of the LIMA graft in conventional CABG of 90% (54,55). Balkhy et al. propose that anastomotic connectors may be instrumental in achieving reproducible long-term patency results in multivessel off-pump TECAB (35).
High rates of conversion have previously been used as a point of criticism against robotic CABG, however this has expectantly decreased over the last two decades with growing experience (11). The rate of conversion to sternotomy as observed in this meta-analysis is now much lower at less than 3%, compared to 10% in published large series from a decade ago (56,57), and 23–33% in TECAB studies a decade before that (7).
As for unexpected results, the reduction in hospital length of stay appears modest when compared to conventional CABG, indicating that realistically patients may still require six-to-seven postoperative days in hospital. However, in high-volume centers, length of stay can be significantly reduced, with patients staying an average of four days (46). While we expect to use fewer blood products with less invasive surgeries, a surprising number of TECAB patients needed blood transfusions and surgical revisions for bleeding, more so than those undergoing RA-MIDCAB. As previously discussed by Kofler et al., this may be a result of the learning curve of different surgeons and the longer operative times given TECAB is technically more challenging (52). Rate of wound infection is another parameter for which sternal-sparing techniques are expected to reduce, and hence has been touted as beneficial for obese patients whom have a high risk of wound complications. Superficial wound infection in this current meta-analysis was observed at a rate ranging from 0.4–6.9% in this pooled meta-analysis which appear equivocal to deep sternal wound infection (DSWI) rates in the literature (58). However, infection of the port or thoracotomy wound may pose relatively lower risk of serious complication compared to DSWI which has a mortality rate of up to 30% (59).
It is important to note that outcomes of robotic CABG derive from a highly selected pool of low-risk patients, whom are relatively younger and have fewer comorbidities, hence comparisons with conventional CABG must be interpreted with caution (46,60). Furthermore, patients undergoing robotic CABG are largely those with single vessel LAD disease that would usually not be considered for conventional CABG (30). Lin et al. therefore compared these two approaches in patients with multi-vessel disease only and found that in real world practice, robotic CABG could be an effective option in patients with fewer clinical complexities (61).
Though the low rate of perioperative complications observed in this pooled meta-analysis is comparable to previous meta-analyses demonstrating the short-term safety and efficacy of these procedures, perioperative complications appeared to occur at a slightly lower rate in RA-MIDCAB compared to TECAB. This may be due to RA-MIDCAB being performed preferentially than TECAB, as it may be safely and efficiently performed even early in a surgeon’s experience (31). Though not analysed in this study, TECAB is also associated with significantly higher hospital costs, the bulk of which lay in operating room equipment such as distal anastomotic devices (24). Nevertheless, the cost of TECAB may be warranted in more complex, multiarterial revascularisation, which although is possible with RA-MIDCAB, has significant complexity with each additional anastomosis (24).
Furthermore, although MIDCAB is already an attractive alternative to conventional CABG and technologically least complex of all minimally invasive CABG procedures, robotic assistance provides 3D telemanipulation that further minimises access trauma of the LIMA harvest by avoiding larger incisions and wider rib spreading (12,62). In a propensity-matched study by Gofus et al. comparing conventional versus robot-assisted MIDCAB, RA-MIDCAB had lower 24-hour post-operative blood loss and potentially faster recovery, however mortality and risk of perioperative complications were comparative (12).
Robotic assistance has also been adopted in HCR, a revolutionary strategy in which a minimally invasive form of bypass grafting is combined with PCI for the treatment of multivessel disease. Studies on robotic HCR show excellent short-term outcomes with no hospital mortality, post-operative MI ranging from 0–3.7%, stroke ranging from 0–1.7% and freedom from reintervention ranging from 73.4–100% in one meta-analysis (63). With careful patient selection, robotic HCR is an attractive strategy that can achieve complete revascularisation whilst integrating the long-term benefit of bypass grafting with less invasiveness of PCI to non-LAD targets (64).
Limitations
All included studies were retrospective and observational in nature resulting in methodological limitations which render firm conclusions difficult to be drawn. As expected from inherent selection bias that cannot be adjusted for by any statistical methodologies, there was considerable statistical heterogeneity observed in the pooling of baseline patient characteristics, which showed that patients undergoing robotic CABG may not be a generalizable cohort. This is partly owed to pooling of outcomes across two and half decades, encompassing several generations of evolution in robotic instruments and surgical technique. Moreover, several larger studies are from high volume, experienced centers and hence their outcomes may also not be generalizable. Results may be confounded by several factors including conversions, hybrid procedures, whether cardiopulmonary bypass was used and whether cases were from the learning curve. Finally, not all articles reported on consecutive patients, which introduces reporting bias in a selected patient population.
Conclusions
Robotic CABG in this pooled meta-analysis is observed to have acceptable perioperative mortality and complication rates reinforcing it as a safe and feasible approach. Overall graft patency, freedom from MACCE and reintervention appear in favour of long-term durability. With a multitude of alternate approaches to coronary bypass grafting in this age, careful patient selection remains paramount for achieving a successful outcome. Robotic CABG, especially TECAB, is the least invasive approach to CABG and has a promising role in HCR, however its continued uptake requires support from both the surgical community and industry alike.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Leonard JR, Rahouma M, Abouarab AA, et al. Totally endoscopic coronary artery bypass surgery: A meta-analysis of the current evidence. Int J Cardiol 2018;261:42-6. [Crossref] [PubMed]
- Bonatti J, Wallner S, Winkler B, et al. Robotic totally endoscopic coronary artery bypass grafting: current status and future prospects. Expert Rev Med Devices 2020;17:33-40. [Crossref] [PubMed]
- Cheng N, Zhang H, Yang M, et al. Eleven-year outcomes of U-clips in totally robotic coronary artery bypass grafting versus standard hand-sewn running suture in robotic-assisted coronary artery bypass grafting. Interact Cardiovasc Thorac Surg 2021;33:27-33. [Crossref] [PubMed]
- Guenther TM, Chen SA, Balkhy HH, et al. Robotic Coronary Artery Bypass Grafting: The Whole 9 Yards. Innovations (Phila) 2020;15:204-10. [Crossref] [PubMed]
- Ekin G, Andrea A, Gianluca T. Robotic Coronary Artery Bypass Grafting: History, Current Technique, and Future Perspectives. In: Serdar K, editor. Latest Developments in Medical Robotics Systems. Rijeka: IntechOpen; 2021:Ch. 5.
- Balkhy HH. Robotic totally endoscopic coronary artery bypass grafting: It's now or never! JTCVS Tech 2021;10:153-7. [Crossref] [PubMed]
- de Cannière D, Wimmer-Greinecker G, Cichon R, et al. Feasibility, safety, and efficacy of totally endoscopic coronary artery bypass grafting: multicenter European experience. J Thorac Cardiovasc Surg 2007;134:710-6. [Crossref] [PubMed]
- Yang M, Wu Y, Wang G, et al. Robotic Total Arterial Off-Pump Coronary Artery Bypass Grafting: Seven-Year Single-Center Experience and Long-Term Follow-Up of Graft Patency. Ann Thorac Surg 2015;100:1367-73. [Crossref] [PubMed]
- Halkos ME, Liberman HA, Devireddy C, et al. Early clinical and angiographic outcomes after robotic-assisted coronary artery bypass surgery. J Thorac Cardiovasc Surg 2014;147:179-85. [Crossref] [PubMed]
- Giambruno V, Chu MW, Fox S, et al. Robotic-assisted coronary artery bypass surgery: an 18-year single-centre experience. Int J Med Robot 2018;14:e1891. [Crossref] [PubMed]
- Göbölös L, Ramahi J, Obeso A, et al. Robotic Totally Endoscopic Coronary Artery Bypass Grafting: Systematic Review of Clinical Outcomes from the Past two Decades. Innovations (Phila) 2019;14:5-16. [Crossref] [PubMed]
- Gofus J, Cerny S, Shahin Y, et al. Robot-assisted vs. conventional MIDCAB: A propensity-matched analysis. Front Cardiovasc Med 2022;9:943076. [Crossref] [PubMed]
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372: [Crossref] [PubMed]
- Institute of Health Economics (IHE). Quality Appraisal of Case Series Studies Checklist. Edmonton (AB): Institute of Health Economics; 2014. Available online: http://www.ihe.ca/research-programs/rmd/cssqac/cssqac-about
- Wan X, Wang W, Liu J, et al. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 2014;14:135. [Crossref] [PubMed]
- Haddaway NR, Page MJ, Pritchard CC, et al. PRISMA2020: An R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Syst Rev 2022;18:e1230. [Crossref] [PubMed]
- Lo CY, Yu CL, Chang Y, et al. Long-term results of robotic-assisted coronary artery bypass grafting with composite arterial grafts for multiple coronary anastomoses: 10-year experience. J Robot Surg 2023;17:63-71. [Crossref] [PubMed]
- Jonsson A, Binongo J, Patel P, et al. Mastering the Learning Curve for Robotic-Assisted Coronary Artery Bypass Surgery. Ann Thorac Surg 2023;115:1118-25. [Crossref] [PubMed]
- Torregrossa G, Sá MP, Van den Eynde J, et al. Robotic-assisted versus conventional off-pump coronary surgery in women: A propensity-matched study. J Card Surg 2022;37:3525-35. [Crossref] [PubMed]
- Piperata A, Busuttil O, Jansens JL, et al. A Single Center Initial Experience with Robotic-Assisted Minimally Invasive Coronary Artery Bypass Surgery (RA-MIDCAB). J Pers Med 2022;12:1895. [Crossref] [PubMed]
- Varrone M, Sarmiento IC, Pirelli L, et al. Minimally Invasive Direct Coronary Artery Bypass: An Evolving Paradigm Over the Past 25 Years. Innovations (Phila) 2022;17:521-7. [Crossref] [PubMed]
- Patrick WL, Iyengar A, Han JJ, et al. The learning curve of robotic coronary arterial bypass surgery: A report from the STS database. J Card Surg 2021;36:4178-86. [Crossref] [PubMed]
- Wu CJ, Chen HH, Cheng PW, et al. Outcome of Robot-Assisted Bilateral Internal Mammary Artery Grafting via Left Pleura in Coronary Bypass Surgery. J Clin Med 2019;8:502. [Crossref] [PubMed]
- Pasrija C, Kon ZN, Ghoreishi M, et al. Cost and Outcome of Minimally Invasive Techniques for Coronary Surgery Using Robotic Technology. Innovations (Phila) 2018;13:282-6. [Crossref] [PubMed]
- Roubelakis A, Casselman F, van der Merwe J, et al. Robotic-enhanced coronary surgery in octogenarians. Interact Cardiovasc Thorac Surg 2017;24:384-7. [Crossref] [PubMed]
- Sabashnikov A, Patil NP, Weymann A, et al. Outcomes after different non-sternotomy approaches to left single-vessel revascularization: a comparative study with up to 10-year follow-up. Eur J Cardiothorac Surg 2014;46:e48-55. [Crossref] [PubMed]
- Bayramoglu Z, Caynak B, Ezelsoy M, et al. Angiographic evaluation of graft patency in robotic-assisted coronary artery bypass surgery: 8 year follow-up. Int J Med Robot 2014;10:121-7. [Crossref] [PubMed]
- Fujita T, Hata H, Shimahara Y, et al. Initial experience with internal mammary artery harvesting with the da Vinci Surgical System for minimally invasive direct coronary artery bypass. Surg Today 2014;44:2281-6. [Crossref] [PubMed]
- Ishikawa N, Watanabe G, Tomita S, et al. Robot-assisted minimally invasive direct coronary artery bypass grafting. ThoraCAB. Circ J 2014;78:399-402. [Crossref] [PubMed]
- Leyvi G, Forest SJ, Srinivas VS, et al. Robotic coronary artery bypass grafting decreases 30-day complication rate, length of stay, and acute care facility discharge rate compared with conventional surgery. Innovations (Phila) 2014;9:361-7; discussion 367. [Crossref] [PubMed]
- Turner WF Jr, Sloan JH. Robotic-assisted coronary artery bypass on a beating heart: initial experience and implications for the future. Ann Thorac Surg 2006;82:790-4; discussion 794. [Crossref] [PubMed]
- Derose JJ Jr, Balaram SK, Ro C, et al. Mid-term results and patient perceptions of robotically-assisted coronary artery bypass grafting. Interact Cardiovasc Thorac Surg 2005;4:406-11. [Crossref] [PubMed]
- Falk V, Diegeler A, Walther T, et al. Total endoscopic computer enhanced coronary artery bypass grafting. Eur J Cardiothorac Surg 2000;17:38-45. [Crossref] [PubMed]
- Balkhy HH, Nisivaco SM, Hashimoto M, et al. Robotic Total Endoscopic Coronary Bypass in 570 Patients: Impact of Anastomotic Technique in Two Eras. Ann Thorac Surg 2022;114:476-82. [Crossref] [PubMed]
- Balkhy HH, Nathan S, Torregrossa G, et al. Angiographic patency after robotic beating heart totally endoscopic coronary artery bypass grafting facilitated by automated distal anastomotic connectors. Interact Cardiovasc Thorac Surg 2020;31:467-74. [Crossref] [PubMed]
- Stastny L, Kofler M, Dumfarth J, et al. Long-Term Clinical and Computed Tomography Angiographic Follow-up After Totally Endoscopic Coronary Artery Bypass Grafting. Innovations (Phila) 2018;13:5-10. [Crossref] [PubMed]
- Zaouter C, Imbault J, Labrousse L, et al. Association of Robotic Totally Endoscopic Coronary Artery Bypass Graft Surgery Associated With a Preliminary Cardiac Enhanced Recovery After Surgery Program: A Retrospective Analysis. J Cardiothorac Vasc Anesth 2015;29:1489-97. [Crossref] [PubMed]
- Dhawan R, Roberts JD, Wroblewski K, et al. Multivessel beating heart robotic myocardial revascularization increases morbidity and mortality. J Thorac Cardiovasc Surg 2012;143:1056-61. [Crossref] [PubMed]
- Jegaden O, Wautot F, Sassard T, et al. Is there an optimal minimally invasive technique for left anterior descending coronary artery bypass? J Cardiothorac Surg 2011;6:37. [Crossref] [PubMed]
- Srivastava S, Gadasalli S, Agusala M, et al. Beating heart totally endoscopic coronary artery bypass. Ann Thorac Surg 2010;89:1873-9; discussion 1879-80. [Crossref] [PubMed]
- Mishra YK, Wasir H, Sharma KK, et al. Totally endoscopic coronary artery bypass surgery. Asian Cardiovasc Thorac Ann 2006;14:447-51. [Crossref] [PubMed]
- Argenziano M, Katz M, Bonatti J, et al. Results of the prospective multicenter trial of robotically assisted totally endoscopic coronary artery bypass grafting. Ann Thorac Surg 2006;81:1666-74; discussion 1674-5. [Crossref] [PubMed]
- Al-Mulla AW, Sarhan HHT, Abdalghafoor T, et al. Robotic Coronary Revascularization is Feasible and Safe: 10-year Single-Center Experience. Heart Views 2022;23:195-200. [Crossref] [PubMed]
- Cerny S, Oosterlinck W, Onan B, et al. Robotic Cardiac Surgery in Europe: Status 2020. Front Cardiovasc Med 2021;8:827515. [Crossref] [PubMed]
- Yokoyama Y, Kuno T, Malik A, et al. Outcomes of robotic coronary artery bypass versus nonrobotic coronary artery bypass. J Card Surg 2021;36:3187-92. [Crossref] [PubMed]
- Whellan DJ, McCarey MM, Taylor BS, et al. Trends in Robotic-Assisted Coronary Artery Bypass Grafts: A Study of The Society of Thoracic Surgeons Adult Cardiac Surgery Database, 2006 to 2012. Ann Thorac Surg 2016;102:140-6. [Crossref] [PubMed]
- Cavallaro P, Rhee AJ, Chiang Y, et al. In-hospital mortality and morbidity after robotic coronary artery surgery. J Cardiothorac Vasc Anesth 2015;29:27-31. [Crossref] [PubMed]
- Casula R, Khoshbin E, Athanasiou T. The midterm outcome and MACE of robotically enhanced grafting of left anterior descending artery with left internal mammary artery. J Cardiothorac Surg 2014;9:19. [Crossref] [PubMed]
- Currie ME, Romsa J, Fox SA, et al. Long-term angiographic follow-up of robotic-assisted coronary artery revascularization. Ann Thorac Surg 2012;93:1426-31. [Crossref] [PubMed]
- Folliguet TA, Dibie A, Philippe F, et al. Robotically-assisted coronary artery bypass grafting. Cardiol Res Pract 2010;2010:175450. [Crossref] [PubMed]
- Mishra YK, Wasir H, Rajneesh M, et al. Robotically enhanced coronary artery bypass surgery. J Robot Surg 2007;1:221-6. [Crossref] [PubMed]
- Kofler M, Stastny L, Reinstadler SJ, et al. Robotic Versus Conventional Coronary Artery Bypass Grafting: Direct Comparison of Long-Term Clinical Outcome. Innovations (Phila) 2017;12:239-46. [Crossref] [PubMed]
- Holm NR, Mäkikallio T, Lindsay MM, et al. Percutaneous coronary angioplasty versus coronary artery bypass grafting in the treatment of unprotected left main stenosis: updated 5-year outcomes from the randomised, non-inferiority NOBLE trial. Lancet 2020;395:191-9. [Crossref] [PubMed]
- Waheed A, Klosterman E, Lee J, et al. Assessing the Long-term Patency and Clinical Outcomes of Venous and Arterial Grafts Used in Coronary Artery Bypass Grafting: A Meta-analysis. Cureus 2019;11:e5670. [Crossref] [PubMed]
- Tinica G, Chistol RO, Enache M, et al. Long-term graft patency after coronary artery bypass grafting: Effects of morphological and pathophysiological factors. Anatol J Cardiol 2018;20:275-82. [Crossref] [PubMed]
- Bonaros N, Schachner T, Lehr E, et al. Five hundred cases of robotic totally endoscopic coronary artery bypass grafting: predictors of success and safety. Ann Thorac Surg 2013;95:803-12. [Crossref] [PubMed]
- Daniel WT, Puskas JD, Baio KT, et al. Lessons learned from robotic-assisted coronary artery bypass surgery: risk factors for conversion to median sternotomy. Innovations (Phila) 2012;7:323-7. [Crossref] [PubMed]
- Ma JG, An JX. Deep sternal wound infection after cardiac surgery: a comparison of three different wound infection types and an analysis of antibiotic resistance. J Thorac Dis 2018;10:377-87. [Crossref] [PubMed]
- Gummert JF, Barten MJ, Hans C, et al. Mediastinitis and cardiac surgery--an updated risk factor analysis in 10,373 consecutive adult patients. Thorac Cardiovasc Surg 2002;50:87-91. [Crossref] [PubMed]
- Seco M, Edelman JJ, Yan TD, et al. Systematic review of robotic-assisted, totally endoscopic coronary artery bypass grafting. Ann Cardiothorac Surg 2013;2:408-18. [Crossref] [PubMed]
- Lin TH, Wang CW, Shen CH, et al. Clinical outcomes of multivessel coronary artery disease patients revascularized by robot-assisted vs conventional standard coronary artery bypass graft surgeries in real-world practice. Medicine (Baltimore) 2021;100:e23830. [Crossref] [PubMed]
- Bonatti J, Wallner S, Crailsheim I, et al. Minimally invasive and robotic coronary artery bypass grafting-a 25-year review. J Thorac Dis 2021;13:1922-44. [Crossref] [PubMed]
- Wang N, Zhou JJ, Phan S, et al. Robot-assisted Hybrid Coronary Revascularisation: Systematic Review. Heart Lung Circ 2015;24:1171-9. [Crossref] [PubMed]
- Aluthman U, Bafageeh SW, Ashour MA, et al. A robotic-assisted hybrid coronary revascularization program: Establishment and early experience in the Middle East. J Card Surg 2022;37:4783-9. [Crossref] [PubMed]






