Aortic valve-sparing procedure in the pediatric population
Introduction
In the early nineties, various valve-sparing procedures were developed and became rapidly mainstream procedures for adults with aortic root aneurysms who had preserved aortic leaflet integrity, mainly Marfan disease and aortic dissection (1). Rapidly, these procedures were brought to the pediatric population (2,3). Primary indications were aortic root aneurysms, in majority Marfan disease and Loeys-Dietz syndrome but also extended to patients with congenital heart disease with dilated aortic roots, namely cono-truncal anomalies such as tetralogy of Fallot and transposition of the great arteries.
The results from these pediatric experiences were discrepant with some reporting disappointing results and some reporting similar outcomes than seen in the adult population (3-6). We hereby report our experience with aortic valve-sparing procedures in the pediatric population.
Methods
We retrospectively reviewed all patients who underwent aortic valve-sparing procedure at the Royal Children’s Hospital, Melbourne, Australia between April 2006 and April 2016. The data was obtained from medical and electronic patient records. Transthoracic echocardiography was performed on all patients to evaluate aortic valve function and proximal aorta dimensions pre- and post-operatively. The echocardiographic data included aortic root diameters, corresponding Z scores, and the degree of aortic regurgitation.
The study was approved by the hospital’s Institutional Review Board, and the requirement for written informed consent was waived due to the observational nature of the study.
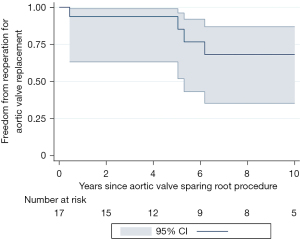
Data was retrospectively analyzed and presented as absolute numbers and percentages for categorical variables and as median values and interquartile ranges for continuous variables, unless otherwise stated. Kaplan-Meier calculations were used for survival analysis. The statistical analysis was performed using Stata/SE version 17 (StataCorp, Texas, USA).
Results
Patient characteristics
Baseline characteristics of the study are shown in Table 1. Of the 17 patients, 14 patients were male (82.4%) and the median age at surgery was 15.7 years [interquartile range (IQR): 12.8–17.4 years] (max/min: 3/19). The most common diagnosis was transposition of great arteries after arterial switch operation (47%, 8/17), followed by Loeys-Dietz syndrome (23.5%, 4/17) and Marfan syndrome (11.8%, 2/17).
Table 1
| Variable | Value (n=17) |
|---|---|
| Sex, male | 82.4 [14] |
| Age, year | 15.7 [12.8–17.4] |
| Weight, kg | 64 [49–70] |
| Diagnosis | |
| Transposition of great arteries, post-arterial switch operation | 47 [8] |
| Loeys-Dietz syndrome | 23.5 [4] |
| Marfan syndrome | 11.8 [2] |
| Tricuspid atresia, Transposition of great arteries, post-arterial switch operation | 5.9 [1] |
| Aortic valve regurgitation, Bicuspid aortic valve | 5.9 [1] |
| Tetralogy of Fallot, post-total repair | 5.9 [1] |
Data are presented as % [n] or median [interquartile range].
Procedure
The David procedure was performed in all 17 patients, with a median cardiopulmonary bypass time of 214 minutes (IQR: 105–252 minutes) and cross-clamp time of 163 minutes (IQR: 152–200 minutes, Table 2). The most common graft sizes were 28 and 30 mm (24 mm, 11.8%; 26 mm, 35.3%; 28 mm, 5.9%; 30 mm, 35.3%; 32 mm, 11.8%). Eleven patients had detailed operation records available. Among them, 63.6% of the patients required central plication to achieve sufficient valve function. One patient required subcommisural annuloplasty, and two patients required cusp resection and cusp extension.
Table 2
| Variable | Value (n=17) |
|---|---|
| Cardiopulmonary bypass time, min | 214 [105–252] |
| Closs clamp time, min | 163 [152–200] |
| Graft size, mm | |
| 24 | 11.8 [2] |
| 26 | 35.3 [6] |
| 28 | 5.9 [1] |
| 30 | 35.3 [6] |
| 32 | 11.8 [2] |
| Additional procedure | n=11 |
| Central plication | 63.6 [7] |
| Subcommisural annuloplasty | 9.1 [1] |
| Cusp resection | 18.2 [2] |
| Cusp extension | 18.2 [2] |
Data are presented as % [n] or median [interquartile range].
Clinical outcomes
The median follow-up period was 9.2 years (IQR: 4.2–10.8 years) and there was no mortality during follow-up (Table 3). Five patients (29.4%) required reoperation and four patients (23.5%) required aortic valve replacement. Ascending aorta and arch replacement were performed in one patient with Loeys-Dietz syndrome a decade after the initial operation. The indication for aortic valve reoperation were recurrence of severe aortic regurgitation. One patient operated at 3.5 years of age had a reoperation within three months for dehiscence of the proximal anastomosis and underwent an aortic homograft root replacement. Freedom from reoperation for aortic valve replacement at 1, 5, 10 years was 93.8%, 93.8% and 68.2% respectively (Figure 1). No incidences of bleeding, thromboembolic events, or subsequent cardiovascular interventions, other than reoperation, were observed during the follow-up period.
Table 3
| Variable | Value (n=17) |
|---|---|
| Follow-up periods, year | 9.2 [4.2–10.8] |
| Mortality | 0 [0] |
| Reoperation | 29.4 [5] |
| Aortic valve replacement | 23.5 [4] |
| Major bleeding | 0 [0] |
| Thrombotic event | 0 [0] |
Data are presented as % [n] or median [interquartile range].
Echocardiography
Pre- and post-operative echocardiography was performed on all 17 patients. More than moderate aortic regurgitation was present preoperatively in 94.1% (16/17) of patients (Table 4). At the last follow-up echocardiography (median postoperative years: 9.2, 4.2–10.8), none of the 13 patients had moderate regurgitation or worse, while 23.5% (4/17) of patients had a mechanical valve.
Table 4
| Variable | Value (n=17) |
|---|---|
| Preoperative sino-tubular junction diameter, mm | 32 [30–34] |
| Preoperative sino-tubular junction diameter, z-score | 4 [2.9–4.4] |
| Preoperative sinus diameter, mm | 46 [40–50] |
| Preoperative sinus diameter, z-score | 6.3 [4.7–6.8] |
| Preoperative annular diameter, mm | 27 [25–28] |
| Preoperative annular diameter, z-score | 3.8 [3.2–4.8] |
| Preoperative aortic regurgitation | |
| None | 0 [0] |
| Trivial | 5.9 [1] |
| Mild | 0 [0] |
| Moderate | 70.6 [12] |
| Severe | 23.5 [4] |
| Last follow-up echo, year | 9.2 [4.2–10.8] |
| Aortic regurgitation | n=13 |
| None | 0 [0] |
| Trivial | 7.7 [1] |
| Mild | 92.3 [12] |
| Moderate | 0 [0] |
| Severe | 0 [0] |
| Mechanical valve | 23.5 [4] |
Data are presented as % [n] or median [interquartile range].
Discussion
While the basic techniques of aortic valve-sparing operations applied in the pediatric population are essentially the same as in the adults, there are important differences in terms of indications, techniques, and outcomes.
Indication for surgery
Aortic root aneurysm without congenital heart disease
The indication of aortic valve-sparing surgery before an adult size is attained at adolescence remains subjected to individual biases of estimates of the severity of the condition. Since most of the indication for this surgery remains based on absolute size estimates, and most pediatric teams interpret sizes in Z-scores, most teams struggle to have a real estimate of the severity of the dilatation of the aortic root. Great differences can also be seen between various teams. Some will extrapolate adult indications based on size and will offer surgery at a level of dilatation that looks equivalent to the adult dilatation. Others, based on the fact that dissection and rupture of the aorta in aortic root aneurysms excluding Loeys Dietz syndrome seems extremely rare before adolescence would postpone surgery to a much more advanced degree of dilatation. Another parameter to consider is the absolute size of the aorta, in particular the aorto-ventricular junction. Keeping in mind the small risk of dissection and rupture, one may want to attempt a valve-sparing operation that would keep its chances to reach adulthood without necessitating the replacement of the Dacron graft by a larger one. We estimate that the bare minimum of the size of the graft that could be large enough for an adult would be a 24 mm graft. Therefore, we have been waiting till the child grows to the point that the aorto-ventricular junction is 21 mm before proceeding to the operation. The mean age of this cohort is 15 years. An earlier threshold will be always kept for patients with Loeys-Dietz syndrome. The youngest child that we have operated was 3 years of age and that threshold seems equivalent to the published literature (3,4).
Another question to be solved at the time of the procedure is whether an intervention should be performed on the arch at the time of aortic valve-sparing procedure or not. Surgeons with the largest experience in Marfan disease have claimed that once the aortic root and the ascending aorta is replaced by prosthetic material, no further progression of the disease is observed on the arch. The situation is different in Loeys-Dietz syndrome where we know that the arch and the origin of the head vessels will ineluctably dilate. When the operation is done very early in life, the size of the arch and the head vessels do not often allow to proceed with the replacement of the arch and the origin of the head vessels. Close observation is then necessary.
Congenital heart disease
We know that patients with tetralogy of Fallot have large aortic root with the root being more dilated if the obstruction to the pulmonary blood flow is more severe (5). We know that a large proportion of patients undergoing the arterial switch have some degree of aortic regurgitation immediately after the procedure, likely because the transfer of the coronary buttons in the neo-aortic root results in aortic root dilatation (6). A small proportion of patients will see a progressive dilatation of the aortic root. Finally, all patients born with a truncus arteriosus will have, by definition, large aortic root after the repair. In all these patients, having a large aortic root becomes an integral part of the condition rather than a pathological status. Rupture and dissection of the aortic root of patients with tetralogy of Fallot, arterial switch operation and truncus have been described but seem to be exceedingly rare (7). Whether or not to reoperate on these patients is often the topic of endless discussion. Common sense may prevail and patients with extremely large aortic root may need to be offered surgery. What many have adopted as a strategy is to serially follow the root size of these patients and operate on those who show a rapid increment of these values.
Adolescent with bicuspid aortic valves
The development of aortic valve repair in the adult population has seen the expansion of aortic valve-sparing operations to serve as a functional annuloplasty of the aortic root in patients with regurgitant bicuspid aortic valve and mild root dilatation. Our experience confirms that performing a repair of a regurgitant bicuspid aortic valve in an adolescent without proper restriction of the annulus lead to a higher rate of failure of the repair. In patients who, often, have more dysplastic valves than adults in their forties or fifties, we have progressively changed our preference for a Ross procedure provided that it can be performed with an inclusion technique, as the longevity of the aortic valve seems superior, the risk of coronary distortion is minimal and the longevity of the right ventricle to pulmonary artery conduit seems to surpass initial expectations.
Techniques
The main challenges of aortic valve-sparing operation in the pediatric population are the intrinsic dysplasia or imposed distortion of the leaflets that makes these lesions among the most challenging to repair.
Size of the graft
In the smallest one of the children undergoing valve-sparing root replacement for aortic root aneurysms, the size of the graft has to be chosen judiciously. For this patient, the smallest graft of the Gelweave Valsalva prosthesis (Terumo, Tokyo, Japan) (26 mm) was selected but was too large for the root, resulting in the dehiscence of the proximal anastomosis. Some selected cases may require the implantation of a straight tube graft of smaller diameters.
Additional leaflet interventions
In our experience, most of these pediatric patients need additional procedures on the leaflets with readjustment of the free length of the leaflets by plication sutures.
Tetralogy of Fallot
One may find that, in tetralogy of Fallot, the left ventricular outflow tract is more deeply embedded within the right ventricular outflow tract making the dissection at that level more challenging. It might be necessary at times, to secure the proximal suture line a little higher up in the interleaflet triangle separating the left from the right coronary sinuses in the same way that is done in the interleaflet triangle separating the right from the non-coronary sinus.
Transposition of the great arteries
The root of the patients who have undergone the arterial switch operation can progressively dilate, leading to aortic regurgitation. The most frequent indication for an operation on the aortic root is by far the presence of increasing regurgitation. It has been well described that up to 35% of the neonates undergoing the arterial switch operation have a new onset of regurgitation after the procedure, even though this regurgitation is usually mild in these early stages of life (8). The likely mechanism of these new onset regurgitation is likely related to the transfer of the coronary buttons in the neo-aortic root, enlarging the sinuses and/or the sino-tubular junction. By the time these patients are discussed for redo surgery, they are usually in the adolescent years or older. All of these patients have suffered from long-standing regurgitation, and we have found a very high incidence of these patients to have, at the time of the redo surgery, not only prolapse of one of the leaflets, but also retraction of some of these cusps. Because of the retraction of the cusps, some of these patients require patch extension of one or more leaflets and we have found aortic valve-sparing surgery more disappointing in this subset of patients.
Outcomes
The results of aortic valve-sparing procedures have been reported to be varied in the literature. Roubertie and colleagues described their experience with 13 patients who underwent aortic valve-sparing procedures, reporting a low rate of freedom from reoperation (54% at 5 years) (9). Patel and colleagues reported on 44 patients with Marfan syndrome and Loeys-Dietz syndrome, with a mean age of ten years. There was no operative mortality, with two late deaths reported (6%). The freedom from aortic valve replacement or repair was 91.7%, 83.3%, and 74.1% at 1-, 3-, and 5-year follow-up after root remodeling (4). Fraser and colleagues reported data from a single institution of 100 consecutive cases of valve-sparing aortic root replacement performed between 1997 and 2017. The overall 1-, 5-, and 10-year survivals were 97%, 97%, and 88%, respectively. The freedom from reintervention with the reimplantation technique at 5 and 10 years was 94.5% and 78.6%, respectively (3). It seems clear that in our experience and those of others, the rate of failure of aortic valve-sparing procedure in the pediatric population is worse than in the adult counterpart with a quarter of these patients facing failure within 5 to 10 years. There may be several reasons for this finding.
One should understand that techniques of aortic valve-sparing operations are often more complex and less easily standardized than in their adult counterparts. Ideally, surgeons should be confident in the practice of aortic valve-sparing surgery in adults before applying these techniques in the pediatric population and be especially proficient in the additional corrective procedures on the leaflets which are often necessary after the root is reconstructed. Once technical barriers are mastered, it seems that aortic valve-sparing procedures in children can provide similar results than those observed in adults provided that the quality of the leaflet tissue is not too severely compromised. Additionally, the aortic valve leaflets of those in the pediatric population seem to be more dysplastic than those found in the adults. In particular, patients who have been subjected to long-standing regurgitation such as those who had arterial switch operations often have retracted thickened leaflets which will be prone to failure.
In conclusion, aortic valve-sparing surgery can be performed in the pediatric population with success but require an experienced surgeon as these valves are often dysplastic or distorted and the aortic valve leaflets require additional procedures.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- David TE, David CM, Manlhiot C, et al. Outcomes of Aortic Valve-Sparing Operations in Marfan Syndrome. J Am Coll Cardiol 2015;66:1445-53. [Crossref] [PubMed]
- Coselli JS, Volguina IV, LeMaire SA, et al. Early and 1-year outcomes of aortic root surgery in patients with Marfan syndrome: a prospective, multicenter, comparative study. J Thorac Cardiovasc Surg 2014;147:1758-66, 1767.e1-4.
- Fraser CD 3rd, Liu RH, Zhou X, et al. Valve-sparing aortic root replacement in children: Outcomes from 100 consecutive cases. J Thorac Cardiovasc Surg 2019;157:1100-9. [Crossref] [PubMed]
- Patel ND, Alejo D, Crawford T, et al. Aortic Root Replacement for Children With Loeys-Dietz Syndrome. Ann Thorac Surg 2017;103:1513-8. [Crossref] [PubMed]
- Niwa K. Aortic root dilatation in tetralogy of Fallot long-term after repair--histology of the aorta in tetralogy of Fallot: evidence of intrinsic aortopathy. Int J Cardiol 2005;103:117-9. [Crossref] [PubMed]
- Prêtre R, Tamisier D, Bonhoeffer P, et al. Results of the arterial switch operation in neonates with transposed great arteries. Lancet 2001;357:1826-30. [Crossref] [PubMed]
- Konstantinov IE, Fricke TA, d'Udekem Y, et al. Aortic dissection and rupture in adolescents after tetralogy of Fallot repair. J Thorac Cardiovasc Surg 2010;140:e71-3. [Crossref] [PubMed]
- Formigari R, Toscano A, Giardini A, et al. Prevalence and predictors of neoaortic regurgitation after arterial switch operation for transposition of the great arteries. J Thorac Cardiovasc Surg 2003;126:1753-9. [Crossref] [PubMed]
- Roubertie F, Ben Ali W, Raisky O, et al. Aortic root replacement in children: a word of caution about valve-sparing procedures. Eur J Cardiothorac Surg 2009;35:136-40. [Crossref] [PubMed]






