Surgical ventricular reconstruction for ischemic cardiomyopathy—a systematic review and meta-analysis of 7,685 patients
Abstract
Background: Surgical ventricular reconstruction (SVR) has been used to control adverse ventricular remodeling and improve cardiac function in ischemic cardiomyopathy. The purpose of this systematic review and meta-analysis was to collect and analyze all available evidence on the utilization and efficacy of SVR.
Methods: An electronic database search was performed to identify all retrospective and prospective studies on SVR for ischemic cardiomyopathy in the English literature from 2000 through 2020. A total of 92 articles with a collective 7,685 patients undergoing SVR were included in the final analysis.
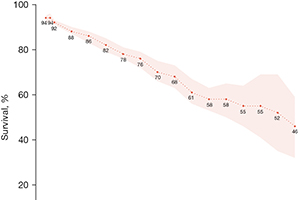
Results: The mean patient age was 61 years (95% CI: 59–63) and 80% (78–82%) were male. Congestive heart failure was present in 66% (54–78%) and angina in 58% (45–70%). Concomitant coronary artery bypass grafting was undertaken in 92% (90–93%) while 21% (18–24%) underwent mitral valve repair. Pre vs. post-SVR, significant improvement was seen in left ventricular ejection fraction (LVEF) [29.9% (28.8–31.2%) vs. 40.9% (39.4–42.4%), P<0.01], left ventricular end-systolic (LVESD) and end-diastolic diameters (LVEDD) [LVESD: 49.9 mm (48.1–51.7) vs. 45 mm (42.8–47.3), P<0.01, LVEDD: 63.8 mm (62–65.6) vs. 58.23 mm (56.6–60), P<0.01], and left ventricular end-systolic (LVESVI) and end-diastolic volume indices (LVEDVI) [LVESVI: 83.9 mL/m2 (79.3–88.4) vs. 46.8 mL/m2 (43.5–50.1), P<0.01; LVEDVI: 119.9 mL/m2 (112.1–127.6) vs. 79.6 mL/m2 (73.6–85.7), P<0.01]. Mean New York Heart Association class improved from 3 (2.8–3.1) to 1.8 (1.5–2) (P<0.01). The 30-day mortality was 4% (3–5%) while late mortality was 19% (9–34%) at a mean follow-up of 27.5 [21–34] months.
Conclusions: In patients with ischemic cardiomyopathy, SVR reduces left ventricular volumes and improves systolic function leading to symptomatic improvement.
Cover