The value of an “Endocarditis Team”
Introduction
Infective endocarditis (IE) is a life-threatening disease with an incidence ranging between 3–10 episodes per 100,000 person-years in various epidemiological studies. It can reach a peak incidence of almost 14.5 episodes per 100,000 person-years in elderly patients (1-3). It can result in major complications and is associated with a high mortality (4,5). It not only affects the heart but can also lead to systemic complications with development of multiorgan dysfunction and sepsis. Despite the acuity of this disease, patients are frequently referred late to specialized centers, commonly after development of significant complications (6-10). Delayed referrals preclude patients from receiving early surgery, sometimes even when indicated (11). A multidisciplinary team approach, which can help in expediting the diagnosis, the decision-making process, and the treatment of patients with IE, gave rise to the concept of the so-called “Endocarditis Team”. Current guidelines for IE provide a Class IIa B recommendation for establishing an Endocarditis Team as a strategy for a collaborative approach to the management of IE (12). Patients with IE should be managed in centers with sufficient resources and adequate infrastructure, because an ideal Endocarditis Team requires the integration of experts from diverse medical fields for implementing appropriate care. The current article addresses multiple aspects related to the Endocarditis Team and highlights its importance for the treatment of patients presenting with IE.
Rationale and evidence for an Endocarditis Team
A collaborative multidisciplinary approach is necessary amongst the members of an Endocarditis Team to manage patients with IE effectively. IE is a complex disease, in which several factors such as underlying cardiac disorders and pre-existing comorbidities, extent of cardiac involvement by infection, systemic spread of the disease with/without multi-organ involvement, the type of causal microorganisms and presence or absence of sepsis or septic shock and/or cardiomyopathy, play an important role in tailoring the management for every patient (12). Early detection of the disease and management before development of complications such as heart failure, peri-annular abscesses, and/or embolic events, are of utmost importance. The prevalence of IE in the general population is low (4,5,12,13). Therefore, general practitioners and low-volume cardiac surgical centers lack adequate experience in the management of such patients. Even in experienced high-volume centers, a single health care provider may not be able to deliver a holistic approach to treatment of such a patient population. A high level of expertise in different areas of clinical medicine is required for comprehensive treatment. Cardiologists, as for most cardiac diseases, are the gatekeepers for the diagnosis of IE. Microbiologists are necessary, not only in identifying the infecting microorganism in blood cultures, but also in determining those existing in valve or myocardial tissue samples procured from the operating room. Infectious disease specialists help implement the most appropriate line of antibiotic therapy based on the blood and tissue culture and sensitivity reports and patient comorbidities such as renal and hepatic dysfunction that may be evident in patients with sepsis or septic shock. Moreover, they can prescribe the most suitable empirical therapy in the absence of blood or tissue culture reports or in the presence of culture-negative endocarditis. Radiologists play an important role throughout the pre- and postoperative management of patients with IE. Even in patients that are conservatively managed, serial radiological investigations are sometimes required to assess the progress of the disease and its response to antibiotic therapy. The first and foremost role of cardiac surgeons is in the decision-making process with respect to the indication and more importantly the timing of surgery. In patients with cerebral complications, such as embolic strokes, intracerebral hemorrhage and/or cerebral abscesses, the opinion of a neurologist or neurosurgeon would also add great value to the process of decision-making. Additionally, general and vascular surgeons and interventionalists are required to manage other embolic complications of IE such as splenic abscesses and peripheral embolism causing mesenteric or femoral artery occlusion. Furthermore, multiple imaging techniques, including echocardiography, magnetic resonance imaging, computed tomography and nuclear imaging are extremely important in the diagnosis, management, decision-making and follow-up of patients with IE (14). Inclusion of all experts from the above-mentioned medical specialties is paramount in establishing a successful Endocarditis Team. Hence, only tertiary or quaternary centers with dedicated multidisciplinary Endocarditis Teams that frequently treat patients with IE would be able to provide high quality care in such patients (13).
The benefit of a multidisciplinary or Heart Team approach in the management, decision-making and therapy selection for patients with heart valve disease and heart failure has been well documented (15-18). Botelho-Nevers et al reported that implementation of a multidisciplinary team approach with standardized medical therapy and surgical indications based on guideline recommendations, reduced 1-year mortality by more than 50% (from 18.2% to 8.2%) (19). They further observed significantly better compliance in antimicrobial therapy and fewer cases of renal failure. Additionally, deaths by embolic events and multiple organ failure syndromes also significantly decreased after the Endocarditis Team was developed. Chirillo and colleagues compared the treatment of IE with and without a multidisciplinary approach and observed a significant reduction in the overall in-hospital (28% vs. 13%, P=0.02) and 3-year mortality (34% vs. 16%, P≤0.001) among operated and conservatively managed patients, and a lower mortality for surgery during the active phase (47% vs. 13%, P≤0.001), favoring the multidisciplinary approach (20). Additionally, fewer patients had culture-negative native valve endocarditis (8% vs. 21%, P=0.01) and worsened renal function (37% vs. 58%, P=0.001) following establishment of the Endocarditis Team. Similarly, a French group implemented weekly multidisciplinary meetings to discuss IE cases. This allowed that facility to adequately follow current guideline recommendations, thus reducing fatality to only 12% despite the increasing complexity of IE cases over time (21). Anguita Sánchez et al. performed a prospective study of IE patients over a period of 15 years. They reported that the adoption of a multidisciplinary treatment strategy during the last years of the study led to an increase in the early elective surgery rates from 22% to 32% (P<0.05), which resulted in a significant reduction in the overall in-hospital mortality from 25% to 12% (P<0.01) (22). The adoption of the Endocarditis Team concept has also been found to be a significant independent predictor of 1-year survival in IE patients (HR 0.24, 95% CI: 0.07 to 0.87; P=0.03) (23). The current guidelines for the management of IE, thereby, strongly recommend the utilization of a specialized team (Endocarditis Team) in the treatment of patients with IE in reference centers (12,24,25).
The Endocarditis Team and reference centers
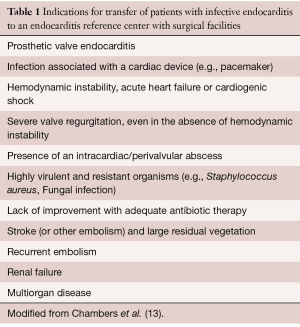
Patients with uncomplicated IE can be initially managed in smaller non-specialized centers, but regular communication with a multidisciplinary Endocarditis Team in reference centers must be established. Therefore, good connectivity should exist between referring hospitals and Endocarditis Teams at reference centers. Lack of improvement or development of complications should prompt immediate transfer of patients to reference centers with an Endocarditis Team (Table 1) (13). Indications that necessitate transfer of patients with IE to reference centers should be clearly laid out by the Endocarditis Team at those centers and should be conveyed to referring hospitals and physicians in the community. Any patient with prosthetic valve endocarditis or infection associated with intra-cardiac devices or catheters should be sent to the reference center sooner than later. Patients with hemodynamic instability, acute heart failure or cardiogenic shock that is commonly caused by acute severe valvular regurgitation or significant intra-cardiac shunts due to endocarditis require emergent surgery to correct the acute mechanical problem and should be immediately transferred to the reference center. Intra-cardiac or peri-annular abscesses can potentially result in intra-cardiac shunts or extra-cardiac rupture or severe para-valvular regurgitation that can lead to sudden hemodynamic instability. Delay in surgery in such patients can lead to further destruction of important adjoining structures, which can deteriorate the general condition of the patient and make an already difficult operation more challenging. Patients who are unresponsive to antibiotic therapy and those presenting with highly virulent organisms such as Staphylococcus aureus, fungi, etc. are at a risk of developing local and systemic complications. Such patients require urgent surgery and should be moved to the reference center as soon as possible. Presence of large vegetations and occurrence of other complications such as stroke, recurrent embolism, renal failure and multi-organ involvement are usually surrogate markers for the severe and advanced disease. Every effort should be made to operate such patients as soon as possible. Reference centers for IE must offer immediate access to diagnostic procedures including transthoracic and transesophageal echocardiography, computed tomography scans, magnetic resonance imaging and nuclear imaging. Additionally, cardiac surgical facility should always be available for patients with complicated IE. The majority of specialist physicians that are involved in the Endocarditis Team such as cardiac surgeons (when possible specialists in valve diseases, congenital heart disease, pacemaker extraction), cardiologists, anesthesiologists, and radiologists should be available at all times in reference centers (12).
Full table
The role of the Endocarditis Team
The role of the Endocarditis Team is multifactorial. It is not only responsible for the management of patients with IE, but also for the educating undergraduate medical students, future clinicians and community health-care workers and undertaking clinical research for quality and safety improvement and reduction of morbidity and mortality observed in patients presenting with this relatively uncommon and potentially deadly disease.
Clinical role
Definitive policies based on national and international guidelines and recommendations should be laid down by the Endocarditis Team at tertiary reference centers in order to promote a standardized management strategy that will translate into high-quality diagnosis and treatment of patients with IE. The physicians involved with the Endocarditis Team should meet on a regular basis to discuss the line of management for new patients and referrals and the ongoing therapy of patients already under treatment in the hospital, to formulate a follow-up plan for patients prior to discharge, to implement new policies or changes in management based on renewed guidelines or important studies and to improve communication and relations with major referring hospitals and clinics.
Most referring centers do not have specialists that have an adequate experience in managing patients with IE and therefore it is difficult or impractical to initiate comprehensive specialist IE care in such hospitals. Hence, it is extremely important to set up a seamless communication between the Endocarditis Team at the reference cardiothoracic center and the referring institutes. It should be easily possible for the Endocarditis Team to establish contact with them, either by e-mail or telephone during work and after-work hours. At the present time, when information technology is easily accessible, telemedicine tools that enable quick sharing of diagnostic imaging and laboratory tests should be made available between the Endocarditis Team at reference centers and as many referring centers and physicians as possible. As mentioned earlier, the Endocarditis Team should prepare a draft that clearly states the criteria for the transfer of patients to the reference center (Table 1). Once the patients have been transferred to the reference center, it is the responsibility of the Endocarditis Team to discuss the complex cases and make decisions regarding the further line of management based on the indications and contraindications for surgery, the optimal timing and type of surgery, if required. Determining the type and the duration of antibiotic therapy to be administered is one of the most important duties of the Endocarditis Team. The timing and necessity of other surgeries that may be essential to treat the focus of infection (e.g., psoas abscess, vertebral body abscess, etc.) or the embolic complications of endocarditis (e.g., splenic, renal or cerebral abscesses) are also the prerogative of the Endocarditis Team.
Apart from this, the Endocarditis Team should ensure that a proper plan has been drawn out for patients following discharge. This is especially imperative for patients who have been conservatively managed, given the risk of progression of valvular disease. The Endocarditis Team in reference centers can facilitate the possibility of providing outpatient parenteral antibiotic treatment, which can help in shortening the length of stay in hospital for selected patients who have otherwise recovered from the surgical trauma and/or the effects of IE (26-28). Substitution of an intravenous antibiotic therapy by an oral one in stable patients with left-sided IE is also a feasible alternative to reduce hospital stay, as was demonstrated by the POET trial (29). The suitability of both above-mentioned alternatives must be discussed within the Endocarditis Team for every patient and selected antibiotic regimes should follow standardized protocols based on current IE guidelines. The frequency of outpatient follow-up visits depends on the patient’s clinical status at discharge from the hospital and should ideally occur at 1, 3, 6, and 12 months after release from the hospital, because the majority of adverse clinical events occur during this period (30). The likelihood of repeat surgery within the first 2 years after discharge is approximately 10% (31). The rate of relapse and recurrence of infection during the first 2 years after discharge is about 8% (31) and 15%, respectively (32-35). Factors associated with increased rates of relapse are summarized in Table 2.

Full table
Furthermore, patients with IE should be educated regarding oral and skin hygiene and preventative dental care as the lack of or inadequate dental surveillance is an important cause of IE (36,37). They should also be informed about their disease as a strategy towards prevention of recurrence and early self-detection of IE, if it does recur. Education about the early detection of recurrent infection could potentially reduce the risk of development of deadly complications, which commonly occur due to a delay in the initiation of appropriate therapy. A film that provides adequate knowledge regarding the important aspects of IE can be shown to the patients prior to discharge and booklets with similar information can be handed over to them at discharge. These are effective means of educating the patients on IE. One of the important functions of the Endocarditis Team is to arrange for rehabilitation of patients who develop IE due to persistent drug abuse.
A clear concept should be developed with regard to the management of recurrent infections in such patients. All the mentioned assignments should be based on standardized protocols according to the current IE guidelines, as non-compliance with guidelines is associated with worse outcomes (10).
Educational role
IE should be part of the curriculum in medical schools by including it as an important component of internal medicine and general surgery syllabus. A series of lectures ought to be conducted for the medical students by various physicians involved in the Endocarditis Team. Additionally, bed-side teaching and visit to the operating rooms to observe surgeries for IE would help in leaving a lasting impression on all students, irrespective of the specialty they choose to pursue in the future. Furthermore, educational material should not only be made available in the form of information booklets for the medical students, but should also be accessible on the hospital website for community physicians and other health-care workers, in an attempt to standardize practice in the community for the management of such patients. Continuous medical educational courses and seminars on IE should be arranged for local health care providers, general practitioners and community cardiologists by the Endocarditis Team so that they remain up-to-date on the latest guidelines in the diagnosis and management of IE. They should be aware of the fact that IE may present as an acute, rapidly progressive infection, or as a subacute or chronic disease that may make the initial diagnosis confusing and misleading. Some patients may present directly with the symptoms of embolic complications such as a stroke, lower limb ischemia, abdominal angina, etc. They should be well informed about the type of patients who are at a higher risk of IE such as those having a prosthetic heart valve or intracardiac devices like pacemakers or automated implantable cardioverter defibrillators, those who have intravenous delivery systems such as ports for chemotherapy or dialysis catheters, those who are immunocompromised, intravenous drug abusers, and those diagnosed with native valvular and/or congenital heart disease. It is extremely important to stress the importance of obtaining blood cultures prior to implementation of antibiotic therapy. The slightest suspicion of IE should immediately prompt the clinician to perform an echocardiography, which not only provides confirmation of the diagnosis but can also predict the risk of embolism and assist in decision-making with respect to the line of management. This would obviously make management of IE efficient and cost-effective, as it would avoid unnecessary transfer of patients who can be managed in peripheral hospitals in consultation with the Endocarditis Team and simultaneously prevent the development of life-threatening complications by enabling early transfer and surgery in patients with appropriate indications for the same. Finally, community physicians should also be made aware of the importance of antibiotic prophylaxis especially in high-risk patients and those who have already undergone surgery for IE.
Research role
Another important responsibility of the Endocarditis Team is the participation in the development and maintenance of clinical data registries on patients with IE. Various teams from the main reference centers should ensure collection of uniform data to evaluate specified outcomes such as early and late mortality, incidence of residual and recurrent endocarditis, freedom from primary surgery or reoperations that serve one or more scientific, clinical, or policy purposes. Registries can be used to determine the indications and optimal timing of surgery when required, the appropriate antimicrobial therapy for complex infections and in comparing different modes of therapy. This would result in quality improvement, clinical research, benchmarking and also indirectly help in developing different payment and reimbursement schemes and models. The information from registries can also be used as a reliable source of information by insurance companies and patients themselves.
Organizing and participating in morbidity and mortality meetings is extremely beneficial in terms of healthcare quality and safety improvement. They are particularly favorable for building teamwork by focusing on constructive criticism rather than accusation. Additionally, such meetings are also very educational for the residents and early career physicians. They also result in policy changes within the hospital and eventually within the community. One study showed that failures in treatment were perceived as a determinant in improving patient safety (38).
Surgery for IE
Antimicrobials can eliminate sensitive microorganisms in blood but cannot penetrate vegetations, abscesses, prosthetic material, especially biofilms that develop on the latter. Delaying surgery could potentially increase the risk of developing local and systemic complications such as septic embolism, valve tissue destruction and invasion of para-valvular structures. Complex reconstructive surgery, which can restore valve function and cardiac integrity, is the only option in the presence of local complications. Systemic involvement through embolism jeopardizes other organ systems, which may make additional surgeries necessary and increase the possibility of development of septic shock, which significantly worsens the outcomes of patients. However, the aim of the Endocarditis Team should be to prevent the development of such complications.
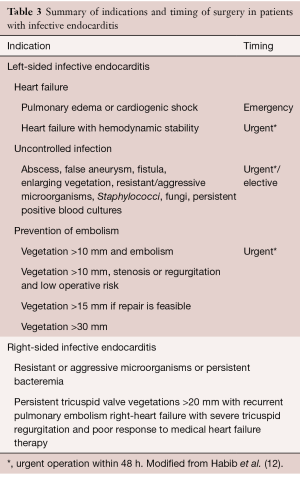
Surgery should be performed sooner than later in patients with large vegetations or intra-cardiac prosthetic material, in whom the risk of embolization or development of perivalvular abscesses is high (8,9,39). Therefore, one of the most important functions of the Endocarditis Team is to determine the correct timing and the type of surgical intervention. Mortality rates are higher in cases of delay in surgery, but may reduce significantly if surgery is performed as soon as the indication has been confirmed (8,9,39). Delaying surgery in hemodynamically stable patients with adequate antimicrobial therapy and an established indication for surgery is not associated with additional benefits (40). Cerebral embolism is not a contraindication for early surgery, however, it is recommended to delay surgery for four weeks in patients with intracerebral hemorrhage, when possible (12,41). In the presence of intracerebral hemorrhage and severe heart failure or cardiogenic shock where delaying surgery is not an option, anticoagulation with nafamostat mesilate, administered in conjunction with low-dose heparin, may be a safe alternative to conventional heparin use during surgery (42). Suggestions from neurologists or neurosurgeons that are a part of the Endocarditis Team are valuable in such situations. Surgical indications as defined in the current guidelines for the management of IE (12,24,25) are summarized in Table 3.
Full table
During surgery, excision of all vegetations and destroyed valvular tissue helps eliminate the sources of embolism. Extensive debridement of all macroscopically infected tissue and total excision of all prosthetic material minimizes the possibility of development of abscesses and residual infections. Nevertheless, antimicrobial therapy still remains the definitive cure of the IE following surgical treatment. Hence, a multifaceted Endocarditis Team would provide better comprehensive patient care than one or two physicians from a single specialty working in isolation.
Another important factor to be considered is the cardiac surgical team. The majority of valve operations for IE can be performed by most trained cardiac surgeons. However, patients with aortic root abscess, intervalvular fibrous body destruction, and rarely involvement of the fibrous skeleton of the heart and those needing valve repairs require the expertise of surgeons that are highly experienced in performing complex reconstructive surgery for IE. Repair is preferable to replacement for the mitral and tricuspid valves, but decision-making regarding repair or replacement may be challenging. Careful judgement needs to be exercised when delaying surgery to potentially increase the possibility of repair as opposed to performing early surgery with valve replacement. The latter often reduces the risk of periannular extension of the infectious process and/or development of heart failure. Prolonged delay in surgery to increase the probability of repair may be counterproductive in certain clinical scenarios and could enhance the risk of irreversible heart damage (43). Apart from surgeons, management of such complex disease also requires highly experienced and knowledgeable anesthesiologists and intensivists capable of treating patients with acute decompensated heart failure, sepsis, and septic cardiomyopathy, who in addition have undergone prolonged complex operative procedures.
Conclusions
Treatment of IE with a multidisciplinary “Endocarditis Team” approach facilitates early diagnosis, implementation of comprehensive therapeutic strategies and appropriate decision-making, which could potentially play an important role in reducing the high morbidity and mortality associated with this disease. Successful execution of such a concept requires a collective effort to optimize communication pathways, to favor inter- and multi-disciplinary approaches, to allow outpatient treatment and follow-up after discharge as well as to strengthen community educational programs and medical training.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Hoen B, Alla F, Selton-Suty C, et al. Changing profile of infective endocarditis: results of a 1-year survey in France. JAMA 2002;288:75-81. [Crossref] [PubMed]
- Hogevik H, Olaison L, Anderson R, et al. Epidemiologic aspects of infective endocarditis in an urban population. A 5-year prospective study. Medicine (Baltimore) 1995;74:324-39. [Crossref] [PubMed]
- Berlin JA, Abrutyn E, Storm BL, et al. Incidence of infective endocarditis in the Delaware Valley 1988-1990. Am J Cardiol 1995;76:933-6. [Crossref] [PubMed]
- Thuny F, Grisoli D, Collart F, et al. Management of infective endocarditis: challenges and perspectives. Lancet 2012;379:965-75. [Crossref] [PubMed]
- Habib G. Management of infective endocarditis. Heart 2006;92:124-30. [Crossref] [PubMed]
- Murdoch DR, Corey R, Hoen B, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med 2009;169:463-73. [Crossref] [PubMed]
- Tornos P, Iung B, Permanyer-Miralda G, et al. Infective endocarditis in Europe: lessons from the Euro heart survey. Heart 2005;91:571-5. [Crossref] [PubMed]
- Delahaye F, Rial MO, de Gevigney G, et al. A critical appraisal of the quality of the management of infective endocarditis. J Am Coll Cardiol 1999;33:788-93. [Crossref] [PubMed]
- Muhlestein JB. Infective endocarditis: how well are we managing our patients? J Am Coll Cardiol 1999;33:794-5. [PubMed]
- González De Molina M, Fernandez-Guerrero JC, et al. Infectious endocarditis: degree of discordance between clinical guidelines recommendations and clinical practice. Rev Esp Cardiol 2002;55:793-800. [PubMed]
- Kiefer T, Park L, Tribouilloy C, et al. Association between valvular surgery and mortality among patients with infective endocarditis complicated by heart failure. JAMA 2011;306:2239-47. [Crossref] [PubMed]
- Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J 2015;36:3075-128. [Crossref] [PubMed]
- Chambers J, Sandoe J, Ray S, et al. The infective endocarditis team: recommendations from an international working group. Heart 2014;100:524-7. [Crossref] [PubMed]
- Bruun NE, Habib G, Thuny F, et al. Cardiac imaging in infectious endocarditis. Eur Heart J 2014;35:624-32. [Crossref] [PubMed]
- Lancellotti P, Rosenhek R, Pibarot P, et al. ESC Working Group on Valvular Heart Disease position paper—heart valve clinics: organization, structure, and experiences. Eur Heart J 2013;34:1597-606. [Crossref] [PubMed]
- Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2017;70:252-89. [Crossref] [PubMed]
- Baumgartner H, Falk V, Bax JJ, et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J 2017;38:2739-91. [Crossref] [PubMed]
- Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur J Heart Fail 2016;18:891-975. [Crossref] [PubMed]
- Botelho-Nevers E, Thuny F, Casalta JP, et al. Dramatic reduction in infective endocarditis-related mortality with a management-based approach. Arch Intern Med 2009;169:1290-8. [Crossref] [PubMed]
- Chirillo F, Scotton P, Rocco F, et al. Impact of a multidisciplinary management strategy on the outcome of patients with native valve infective endocarditis. Am J Cardiol 2013;112:1171-6. [Crossref] [PubMed]
- Camou F, Dijos M, Barandon L, et al. Management of infective endocarditis and multidisciplinary approach. Med Mal Infect 2019;49:17-22. [Crossref] [PubMed]
- Anguita Sánchez M, Torres Calvo F, Castillo Domínguez JC, et al. Short- and long-term prognosis of infective endocarditis in non-injection drug users: improved results over 15 years (1987-2001). Rev Esp Cardiol 2005;58:1188-96. [PubMed]
- Kaura A, Byrne J, Fife A, et al. Inception of the ‘endocarditis team’ is associated with improved survival in patients with infective endocarditis who are managed medically: findings from a before-and-after study. Open Heart 2017;4:e000699. [Crossref] [PubMed]
- AATS Surgical Treatment of Infective Endocarditis Consensus Guidelines Writing Committee Chairs, Pettersson GB, Coselli JS, et al.. 2016 The American Association for Thoracic Surgery (AATS) consensus guidelines: Surgical treatment of infective endocarditis: Executive summary. J Thorac Cardiovasc Surg 2017;153:1241-1258.e29. [Crossref] [PubMed]
- Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientifi c statement for healthcare professionals from the American Heart Association. Circulation 2015;132:1435-86. [Crossref] [PubMed]
- Tice AD, Rehm SJ, Dalovisio JR, et al. Practice guidelines for outpatient parenteral antimicrobial therapy. IDSA guidelines. Clin Infect Dis 2004;38:1651-72. [Crossref] [PubMed]
- Cervera C, del Rio A, Garcia L, et al. Efficacy and safety of outpatient parenteral antibiotic therapy for infective endocarditis: a ten-year prospective study. Enferm Infecc Microbiol Clin 2011;29:587-92. [Crossref] [PubMed]
- Andrews MM, von Reyn CF. Patient selection criteria and management guidelines for outpatient parenteral antibiotic therapy for native valve infective endocarditis. Clin Infect Dis 2001;33:203-9. [Crossref] [PubMed]
- Iversen K, Ihlemann N, Gill SU, et al. Partial Oral versus Intravenous Antibiotic Treatment of Endocarditis. N Engl J Med 2019;380:415-24. [Crossref] [PubMed]
- Thuny F, Giorgi R, Habachi R, et al. Excess mortality and morbidity in patients surviving infective endocarditis. Am Heart J 2012;164:94-101. [Crossref] [PubMed]
- Castillo JC, Anguita MP, Ramirez A, et al. Long term outcome of infective endocarditis in patients who are not drug addicts: a 10 year study. Heart 2000;83:525-30. [Crossref] [PubMed]
- Netzer RO, Altwegg SC, Zollinger E, et al. Infective endocarditis: determinants of long term outcome. Heart 2002;88:61-6. [Crossref] [PubMed]
- Welton DE, Young JB, Gentry WO, et al. Recurrent infective endocarditis. Am J Med 1979;66:932. [Crossref] [PubMed]
- Renzulli A, Carozza A, Romano GP, et al. Recurrent infective endocarditis: a multivariate analysis of 21 years of experience. Ann Thorac Surg 2001;72:39-43. [Crossref] [PubMed]
- Tornos MP, Permanyer-Miralda G, Olona M, et al. Long-term complications of native valve infective endocarditis in non-addicts. A 15-year follow-up study. Ann Intern Med 1992;117:567-72. [Crossref] [PubMed]
- Chambers JB, Dayer M, Prendergast BD, et al. Beyond the antibiotic prophylaxis of infective endocarditis: the problem of dental surveillance. Heart 2013;99:363-4. [Crossref] [PubMed]
- Thornhill MH, Dayer MJ, Forde JM, et al. Impact of the NICE guideline recommending cessation of antibiotic prophylaxis for prevention of infective endocarditis: before and after study. BMJ 2011;342:d2392. [Crossref] [PubMed]
- Lecoanet A, Vidal-Trecan G, Prate F, et al. Assessment of the contribution of morbidity and mortality conferences to quality and safety improvement: a survey of participants’ perceptions. BMC Health Serv Res 2016;16:176. [Crossref] [PubMed]
- Thuny F, Beurtheret S, Mancini J, et al. The timing of surgery influences mortality and morbidity in adults with severe complicated endocarditis: a propensity analysis. Eur Heart J 2011;32:2027-33. [Crossref] [PubMed]
- Kang DH, Kim YJ, Kim SH, et al. Early surgery versus conventional treatment for infective endocarditis. N Engl J Med 2012;366:2466-73. [Crossref] [PubMed]
- Piper C, Wiemer M, Schulte HD, et al. Stroke is not a contraindication for urgent valve replacement in acute infective endocarditis. J Heart Valve Dis 2001;10:703-11. [PubMed]
- Sakamoto T, Kano H, Miyahara S, et al. Efficacy of nafamostat mesilate as anticoagulation during cardiopulmonary bypass for early surgery in patients with active infective endocarditis complicated by stroke. J Heart Valve Dis 2014;23:744-51. [PubMed]
- Iung B, Rousseau-Paziaud J, Cormier B, et al. Contemporary results of mitral valve repair for infective endocarditis. JACC 2004;43:386-92. [Crossref] [PubMed]






