Comparison of Dacron ring and suture annuloplasty for aortic valve repair—a porcine study
Abstract
Background: A subvalvular annuloplasty is often used for aortic valve repair in patients with isolated aortic regurgitation with aortic annulus dilatation. Our aim was to characterize and compare annulus geometry and dynamics of the Dacron ring and suture annuloplasty and compare it with the native aortic annulus under standardized conditions.
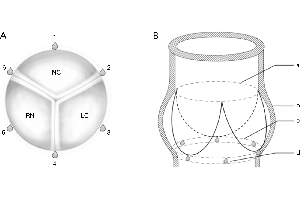
Methods: We randomized 29 pigs of 80 kg into a Dacron ring group, a suture annuloplasty group and a native control group. The assessment was performed using sonomicrometry crystals for evaluation of dynamic geometry, and pressure measurements and echocardiography to evaluate valve performance.
Results: Aortic annulus area (AAA) was significantly reduced in the Dacron and Suture group compared with the Native group. Expansibility was similar and within normal physiologic limits in all three groups (Native: 12%±7%; Dacron: 11%±3%; Suture: 10%±4%). The largest segmental expansion was observed at the right coronary sinus (RC) in the Native and Dacron group but in the Suture group there was no significant difference between segments. The aortic annulus was primarily oval in systole and became more circular in diastole in the Native and Dacron group, however, in the Suture group, the sphericity remained relatively unchanged throughout the cardiac cycle.
Conclusions: This study is the first to describe and compare detailed segmental geometry of the Dacron ring and suture annuloplasty in a standardized porcine model. The two annuloplasties effectively downsized the aortic annulus, while expansibility was maintained. Each annuloplasty had its own geometrical characteristics, but the Dacron ring was more similar to the native aortic annulus than the suture annuloplasty. This study suggests that the Dacron ring offers a more physiological and standardized support by mimicking the geometry and dynamics of the native aortic annulus and thus is a preferable choice over the suture annuloplasty for valve-sparing aortic root procedures.
Cover