Percutaneous coronary intervention versus coronary bypass surgery for unprotected left main disease: a meta-analysis of randomized controlled trials
Introduction
The best option for the treatment of patients with disease of the left main coronary artery is controversial.
Traditionally, left main disease (LMD) has been considered an indication for surgery (1). However, last year the publications of the NOBLE and EXCEL trials, which respectively denied and supported the non-inferiority of percutaneous coronary intervention (PCI) compared to coronary artery bypass grafting (CABG) for LMD, have fueled the debate, adding uncertainty with respect to what the optimal strategy of revascularization for the treatment for patients with unprotected LMD should be.
Herein we perform a meta-analysis of the randomized trials that compare the two treatment options. We also evaluate the effect of the evolution in stent types and SYNTAX (SYNergy between PCI with TAXUS and Cardiac Surgery) score on outcomes.
Methods
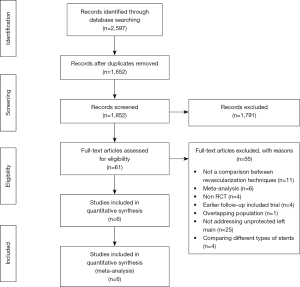
This meta-analysis was performed in accordance with the Meta-Analysis of Observational Studies in Epidemiology (MOOSE) guidelines (Table S1) and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (2,3).

Full table
Data sources and searches
PubMed, EMBASE and the Cochrane Central Register of Controlled Trials were searched from inception to November 2016, without language restrictions. Search terms were “left main” AND (“coronary artery bypass” OR CABG OR “bypass surgery” OR “coronary bypass”) AND (“percutaneous coronary intervention” OR “PCI” OR “stent”). Reference lists of the identified articles and relevant reviews and meta-analyses were screened by 2 reviewers (A Di Franco, LB Ohmes) to identify any additional relevant studies (i.e., backward snowballing).
Study selection
Investigators examined references at the title/abstract level, with divergences resolved by consensus, and then, if any potentially pertinent title/abstract was found, the complete article was retrieved. All articles with random allocation to treatment, comparing CABG to PCI with stents for unprotected LMD, were included.
Data extraction and quality assessment
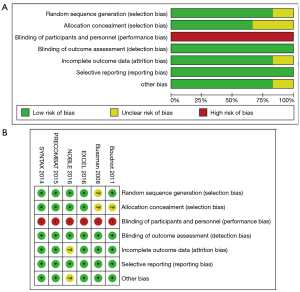
Baseline data including SYNTAX score (4), procedural outcome, and follow-up time were independently abstracted by two investigators (A Di Franco, LB Ohmes). Outcomes were analyzed according to the intention-to-treat principle. Outcomes were adjudicated according to the original authors’ definitions. Risk of bias among included trials was appraised by two independent investigators (LB Ohmes and M Rahouma) based on the “risk of bias assessment tool” provided by the Cochrane collaboration (5), in which 7 domains were assessed for each randomized controlled trial (RCT): random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessors (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and presence of other bias. The presence of a possible source of bias in each domain was assessed, and a final judgment of low, unclear, or high risk of bias was assigned.
Outcomes
The primary outcome was a composite of follow-up death/myocardial infarction/stroke/repeat revascularization at the longest available follow-up. The secondary outcomes were peri-procedural mortality, and the individual components of the primary outcome.
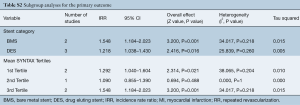
For the primary outcome, two different subgroup analyses were conducted based on: (I) type of stents used in the PCI group [bare metal stents (BMS) vs. drug-eluting stents (DES)]; and (II) tertiles of mean SYNTAX score. The cut-offs for 1st and 2nd tertiles were 22.80 and 25.05, respectively.
Data synthesis and analysis
This pairwise meta-analysis was conducted using Comprehensive Meta-Analysis (CMA) V 3.0 (2006 Biostat, Inc, Englewood, NJ, USA). Review Manager (RevMan) 5.3 was used for risk of bias assessment (6).
Relative effect estimates were calculated as log incidence rate ratios (IRRs) or odds ratio (OR) with 95% confidence intervals (95% CIs). We pooled late outcomes as natural logarithm of the IRR to account for potentially different follow-up durations between different treatments. We estimated the IRR through different means depending on the available study data. When hazard ratios (HRs) were reported, we took the natural logarithm of the HR with standard error (SE) calculated from the 95% CI or log rank P value (7). When Kaplan Meier (K-M) curves were present, event rates were estimated from the curves using GetData Graph Digitizer software 2.26 (http://getdata-graph-digitizer.com/) and in case of absence of K-M curves, we used the reported event rates to calculate the IRR, as previously described (8,9).
IRRs were pooled using the generic inverse variance method with random model. As per guidelines, we reported heterogeneity as: low (I2=0–25%), moderate (I2=26–50%) and high (I2>50%) (5). In all comparisons, the CABG group was used as reference.
For the primary outcome, leave-one-out analysis and funnel plot with trim and fill method to assess for publication bias were performed. Visual inspection and Egger’s test were used to assess for funnel asymmetry (10). Meta-regression was used to assess any association between the primary outcome and female gender, mean age, diabetes and mean SYNTAX score.
Results
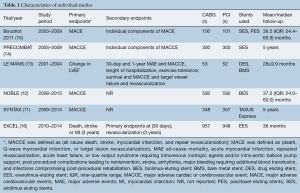
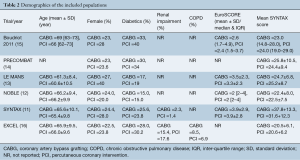
Among 2,597 potentially relevant articles, 6 met the inclusion criteria and were included in the final analysis (11-16). A PRISMA flow chart of study selection is shown in Figure 1. An overview of the included articles is shown in Tables 1,2. Risk of bias assessment for each trial is shown in Figure S1.
Full table
Full table
In total, 4,700 patients were included (2,349 PCI and 2,351 CABG). Follow-up ranged from 2.33 to 5 years.
Primary outcome
PCI was associated with higher risk of follow-up death/myocardial infarction/stroke/repeat revascularization (IRR =1.328, 95% CI, 1.114–1.582, P=0.002) (Figure 2).
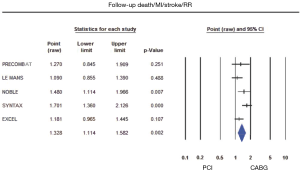
Leave-one-out analysis and funnel plot with trim and fill method for the primary outcome are shown in Figure S2. Egger’s test intercept was 0.277 (95% CI, −11.22–11.77, P=0.944).

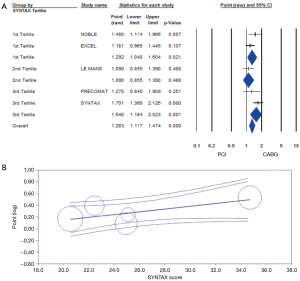
At meta-regression, higher mean SYNTAX score was associated with higher risk of the primary outcome in the PCI group (beta =0.02, P=0.05). No association was found with female gender (beta =−0.01, P=0.70), mean age (beta =0.05, P=0.31), and diabetes (beta =−0.02, P=0.36) (Figure S3). At subgroup analysis based on stents category, PCI was associated with higher risk of the primary outcome both in the BMS (IRR =1.548, 95% CI, 1.184–2.023, P=0.001) and DES (IRR =1.218, 95% CI, 1.038–1.430, P=0.016) subgroups. At subgroup analysis based on tertiles of mean SYNTAX category, PCI was associated with progressively higher risk of the primary outcome in the 1st and 3rd SYNTAX tertile subgroups (IRR =1.292, 95% CI, 1.040–1.604, P=0.021 and IRR =1.548, 95% CI, 1.184–2.023, P=0.001) (Figure 3, Table S2).

Full table
Secondary outcomes
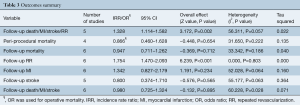
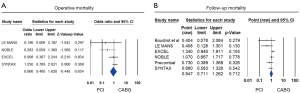
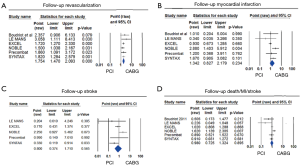
A summary of the outcomes is given in Table 3. No difference between PCI and CABG were found for peri-procedural mortality (OR =0.866, 95% CI, 0.460–1.628, P=0.654), follow-up mortality (IRR =0.947, 95% CI, 0.711–1.262, P=0.712), myocardial infarction (IRR =1.342, 95% CI, 0.827–2.179, P=0.234), or stroke (IRR =0.800, 95% CI, 0.374–1.710, P=0.565). PCI was associated with a higher risk of repeated revascularization (IRR =1.754, 95% CI, 1.470–2.093, P<0.001) (Figures 4,5).
Full table
Discussion
According to the current North American and European Guidelines for the treatment of unprotected LMD, CABG is a class I recommendation whereas PCI is class IIa/III recommendation, depending on the SYNTAX score (1,17). Last year, the publication of two independent randomized trials (the EXCEL and NOBLE trials) (12,16) with opposite results fueled the debate on the best therapeutic strategy for the treatment of LMD. As detailed elsewhere (18), the two studies have very important differences in design, follow-up and outcomes definitions and this is the most likely explanation for the divergence in their conclusions.
In this meta-analysis, we pooled aggregate data from 6 trials totaling 4,700 patients randomized to CABG or PCI. We found that at a mean follow-up ranging from 2.33 to 5 years, PCI was associated with a significantly higher risk of a composite of death/myocardial infarction/stroke/repeat revascularization. This difference was clearly driven by the higher need for repeat revascularization in the PCI arm. No difference in the other individual components of the composite outcome were in fact found. Of note, these findings are in accordance with recent data from Palmerini et al. (19), who showed that PCI, as compared to CABG for treatment of unprotected LMD, while associated with a similar long-term composite risk of death, myocardial infarction, or stroke (HR =1.06, 95% CI, 0.82–1.37), is also associated with greater rates of unplanned revascularization (HR =1.74, 95% CI, 1.47–2.07).
Interestingly, the introduction of new generation DES did not shift the results in favor of PCI, as shown in our subgroup analysis. Recent evidence from our group elicit the doubt that new generation DES could have significantly worse results in the treatment of LMD, as suggested by the fact that second-generation DES, but not BMS, and first-generation DES were associated with a significantly increased risk of death/myocardial infarction/stroke when compared with CABG (20).
Another important finding is that the advantage for the CABG group in terms of primary outcome is independent of SYNTAX score, although it is progressively more evident in the 1st and 3rd SYNTAX score tertile subgroups (IRR =1.292, 95% CI, 1.040–1.604, P=0.021 and IRR =1.55, 95% CI, 1.184–2.023, P=0.001).
Finally, unique to our report, as compared to prior works on the topic (19), is the fact that we were able to demonstrate that results were not affected by age, gender or diabetes.
This study shares the limitations of aggregate data analyses. The included trials were performed in different years, by different institutions using different protocols and definitions and some degree of heterogeneity is very likely to exist. Also, procedural aspects of both PCI and CABG (type of stents, use of arterial grafts or off-pump technique) varied considerably between different studies. Finally, meta-regression analyses can be viewed only as exploratory in this setting.
In conclusion, our results support the concept that CABG remains the therapy of choice for the treatment of unprotected LMD, especially for patients with high SYNTAX score.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Hillis LD, Smith PK, Anderson JL, et al. 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2011;124:e652-735. [Crossref] [PubMed]
- Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008-12. [Crossref] [PubMed]
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. [Crossref] [PubMed]
- Yadav M, Palmerini T, Caixeta A, et al. Prediction of coronary risk by SYNTAX and derived scores: synergy between percutaneous coronary intervention with taxus and cardiac surgery. J Am Coll Cardiol 2013;62:1219-30. [Crossref] [PubMed]
- Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [Crossref] [PubMed]
- Review Manager (RevMan). Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 2014.
- Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med 1998;17:2815-34. [Crossref] [PubMed]
- Yanagawa B, Verma S, Jüni P, et al. A systematic review and meta-analysis of in situ versus composite bilateral internal thoracic artery grafting. J Thorac Cardiovasc Surg 2017;153:1108-16.e16. [Crossref] [PubMed]
- Tierney JF, Stewart LA, Ghersi D, et al. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 2007;8:16. [Crossref] [PubMed]
- Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-34. [Crossref] [PubMed]
- Morice MC, Serruys PW, Kappetein AP, et al. Five-year outcomes in patients with left main disease treated with either percutaneous coronary intervention or coronary artery bypass grafting in the synergy between percutaneous coronary intervention with taxus and cardiac surgery trial. Circulation 2014;129:2388-94. [Crossref] [PubMed]
- Mäkikallio T, Holm NR, Lindsay M, et al. Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): a prospective, randomised, open-label, non-inferiority trial. Lancet 2016;388:2743-52. [Crossref] [PubMed]
- Buszman PE, Kiesz SR, Bochenek A, et al. Acute and late outcomes of unprotected left main stenting in comparison with surgical revascularization. J Am Coll Cardiol 2008;51:538-45. [Crossref] [PubMed]
- Ahn JM, Roh JH, Kim YH, et al. Randomized trial of stents versus bypass surgery for left main coronary artery disease: 5-year outcomes of the PRECOMBAT study. J Am Coll Cardiol 2015;65:2198-206. [Crossref] [PubMed]
- Boudriot E, Thiele H, Walther T, et al. Randomized comparison of percutaneous coronary intervention with sirolimus-eluting stents versus coronary artery bypass grafting in unprotected left main stem stenosis. J Am Coll Cardiol 2011;57:538-45. [Crossref] [PubMed]
- Stone GW, Sabik JF, Serruys PW, et al. Everolimus-Eluting Stents or Bypass Surgery for Left Main Coronary Artery Disease. N Engl J Med 2016;375:2223-35. [Crossref] [PubMed]
- Authors/Task Force members, Windecker S, Kolh P, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 2014;35:2541-619. [Crossref] [PubMed]
- Gaudino MFL, Ruel M, Taggart DP, et al. Blaise Pascal and the evidence on the use of multiple arterial grafts for coronary artery bypass surgery after the interim analysis of the Arterial Revascularization Trial. Curr Opin Cardiol 2018;33:245-8. [PubMed]
- Palmerini T, Serruys P, Kappetein AP, et al. Clinical outcomes with percutaneous coronary revascularization vs. coronary artery bypass grafting surgery in patients with unprotected left main coronary artery disease: A meta-analysis of 6 randomized trials and 4,686 patients. Am Heart J 2017;190:54-63. [Crossref] [PubMed]
- Benedetto U, Taggart DP, Sousa-Uva M, et al. New generation stents compared to coronary bypass surgery for unprotected left main disease: A word of caution. J Thorac Cardiovasc Surg 2018;155:2013-9.e16. [Crossref] [PubMed]