Management of laryngotracheal trauma
Introduction
One of the earliest accounts of airway trauma was written in 1873 by Seuvre, describing a woman who was crushed by a wagon wheel and was subsequently found to have avulsion of the right mainstem bronchus on autopsy (1). Rudolf Nissen performed the first pneumonectomy in 1931 on a 12-year-old girl who had sustained a crush injury to the thorax. She initially presented with a left-sided tension pneumothorax due to a tear in the left mainstem bronchus. The pneumothorax was decompressed and she subsequently developed chronic pulmonary suppuration and bronchiectasis over the next several months due to bronchostenosis that had developed at the site of the tear. Pneumonectomy was performed in two stages. The first operation was halted because the patient went in to asystole when traction was applied to the hilum of the lung. The completion operation was performed fourteen days later, and the girl lived for many years in excellent physical condition (2).
Laryngotracheal trauma continues to be a rare entity, and accounts for only 1 in every 30,000 emergency room visits in the United States. It is the second most common cause of death in patients with head and neck trauma after intracranial injury (3). Only 0.5% of multiple trauma patients were reported to have injury to the airway at any level. The low incidence of injury to the larynx is likely due to its protected position, by the mandible superiorly, the sternum inferiorly, and the spine posteriorly. In addition, muscular and tendinous attachments to the larynx can deflect trauma in all directions except posteriorly. Laryngeal injuries are therefore often missed due to their infrequency and resultant low clinical suspicion. One retrospective study from Tulane University found that the overall mortality for patients that sustain injury to the tracheobronchial tree was 17%, with the mortality of trauma to the cervical trachea reported as 14% (4).
Mechanism of injury
Blunt trauma is by far the most common mechanism of tracheal injury. The largest review of blunt airway trauma looked at 265 patients over 123 years and unsurprisingly found that the predominant mechanism was following a motor vehicle collision (59%) (5). This usually occurs when the driver’s extended neck hits the steering wheel, dashboard, or windshield. Fortunately, the frequency of these injuries has declined due to the presence of airbags, increased use of seatbelts, and improved dashboard designs. Other mechanisms of blunt injury include crush injury, during sports, in particular ice hockey, basketball, or karate, and as a result of hanging or strangulation (6). Penetrating injuries are much less common and are usually due to stab or bullet wounds. Iatrogenic injuries are extremely uncommon and may occur during percutaneous tracheostomy, unskilled or emergent intubation, or bronchoscopy.
Presentation
Presenting symptoms include dyspnea, dysphonia, hoarseness, stridor, neck pain, dysphagia, and hemoptysis. Physical exam findings may include tenderness over the larynx, subcutaneous emphysema, cyanosis, air escaping from a neck wound, large air leak after chest tube placement, or persistent pneumothorax despite chest tube placement. It is important to remember that the severity of symptoms does not always correspond with the extent of injury (7).
Diagnosis
After the airway has been stabilized, a complete trauma assessment must be performed to assess the degree of injury to the airway and evaluate for other organ injuries due to the high probability of concurrent injuries associated with laryngeal trauma. This evaluation usually begins with a chest X-ray in the trauma bay that may show a pneumothorax, pneumomediastinum, subcutaneous emphysema, or tracheal deviation. A CT scan of the neck and chest is indicated in stable patients and can diagnose most laryngeal fractures and dislocations, as well as identify associated injuries. The esophagus is the most common site of associated injury in tracheobronchial trauma. There is also a high incidence of associated recurrent laryngeal nerve injury in patients with fracture of the cricoid cartilage because of the close proximity to the nerve. Injury to major vessels and the thyroid gland are also commonly seen. CT angiogram may also be indicated if there is suspicion for concomitant vascular injury. One series that investigated major vascular injuries associated with tracheobronchial injuries found that the carotid artery is the most commonly injured vessel (4).
Direct visualization with flexible fiberoptic laryngoscopy and bronchoscopy is very important in diagnosing airway injury at any level. Wherever possible, evaluation of the larynx should be done by an Otolaryngologist (7). Rigid bronchoscopy is usually not needed. It is important to remember to pull back the endotracheal tube in an intubated patient to allow examination of the entire airway. Esophagoscopy and barium swallow should be obtained in patients with a suspected esophageal injury. MRI and MRA currently have no role in the evaluation of laryngotracheal trauma.
Classification
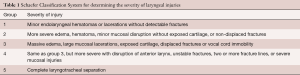
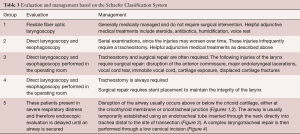
There have been many proposed classifications for laryngeal trauma that categorize injuries according to site (supraglottic, glottic, subglottic), tissues injured (cartilage, mucosa, ligaments, nerves, joints), and severity. The American Academy of Otolaryngology-Head and Neck Surgery has accepted the Schaefer Classification System as the most useful since it allows the clinician to make treatment decisions based on severity of injury (Table 1) (8).
Full table
Management
Every laryngeal injury is unique and the management can therefore be complex. The immediate goal is always to obtain and maintain a stable airway. Patients with respiratory distress or increasing stridor should be intubated immediately, and one should have a low threshold to intubate with the aid of a fiber optic bronchoscope. Minor endolaryngeal lacerations, hematomas and abrasions may be observed for signs of airway compromise.
Airway rupture extending beyond the carina requires placement of an endotracheal tube under bronchoscopic visualization into the mainstem bronchus opposite to the side of the injury to provide single lung ventilation, and insertion of a bronchial blocker as well as a thoracostomy tube on the side of the injury to maintain adequate tidal volumes and prevent the development of tension pneumothorax. Once the airway is secured, further diagnostic workup can commence. Overall management depends on the mechanism, site of injury, and presence of associated injuries.
Hyoid bone
Hyoid bone fractures are rare, and are usually a result of strangulation, sports, or motor vehicle accidents. In a review of 46 patients that sustained hyoid bone fractures, only five underwent surgical repair of the hyoid bone. Fifteen patients required tracheostomy and surgical intervention for related injuries. Most patients were treated with voice rest, diet changes and symptomatic analgesia and both surgical and non-operative management yielded positive patient outcomes with resolution of symptoms (9). Therefore, nonsurgical management of a fractured hyoid bone is the most common method of treatment. If pain over the fractured hyoid persists, some groups advocate excising the bone on either side of the fracture to prevent crepitus (6).
Thyroid cartilage
The thyroid and cricoid cartilages ossify during early childhood, therefore the age of the patient can influence the pattern of injury. A calcified laryngeal complex in an older patient may fracture in more than one place, whereas a more elastic larynx will usually fracture at a single site in a younger person. Fracture occurs when the thyroid cartilage is forced against the cervical spine, flattens, and springs back into position, resulting in an anterior linear fracture down the thyroid prominence (6).
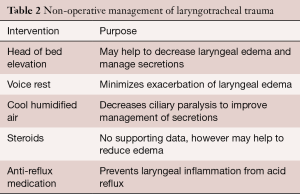
Non-displaced fractures of the thyroid cartilage that have no evidence of internal derangement on endoscopy can be managed non-operatively with supportive measures (Table 2).
Full table
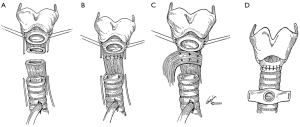
All displaced fractures of the thyroid cartilage should undergo open reduction via a low cervical thyroidectomy incision and should be realigned with a miniplate, wire, or non-absorbable monofilament suture. Miniplate fixation was shown to be superior to suture or wire fixation because it promotes complete cartilaginous union, whereas the latter two methods promote healing by fibrous union (10). The external perichondrium of the cartilage should always be re-approximated. Closed reduction of small fractures or arytenoid dislocations followed by endoscopic placement of an airway stent has been trialed, however the experience is limited with unfavorable results (3). Therefore, surgical intervention should be done via an open procedure.
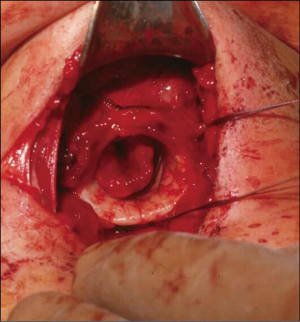
If there is also evidence of internal derangement on pre-operative endoscopy, such as an avulsed vocal cord or displaced epiglottis, this must be repaired after the cartilage to ensure that a proper scaffold is obtained before re-aligning the mucosa. The laryngeal lumen can be accessed either through the fracture itself or via a laryngofissure midline incision through the thyroid cartilage. Mucosal defects are repaired with absorbable suture and buried knots to prevent granuloma formation. If there is extensive mucosal loss, free grafts from the buccal mucosa, skin or dermis may be used to fix the defect.
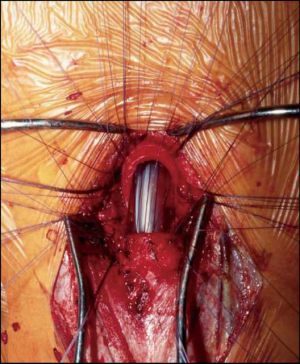
Cricoid cartilage
Injury to the cricoid cartilage is often associated with a fractured thyroid cartilage. Since the cricoid is a complete ring, it usually fractures in two places, anteriorly and posteriorly. Non-displaced, stable fractures can be managed non-operatively. If the fractured segments are unstable, the cartilage should be wired and a soft stent, such as silicone, should be inserted and kept in place for 4–6 weeks. Patients with crushed cricoid rings should have a tracheostomy placed on presentation and the cricoid should be excised in a delayed fashion once the surrounding edema has improved. This usually only requires excision of the anterior half of the cartilage, which can be replaced with a hyoid bone or rib graft.
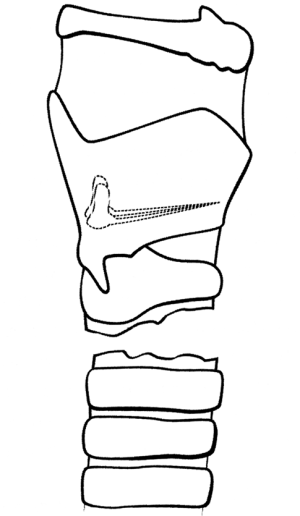
Stents
Airway stents are often placed in the setting of massive endolaryngeal injury to prevent mucosal adhesions and laryngeal stenosis. Another indication for use is for laryngeal injuries in which the anterior commissure is disrupted. Stent placement helps to maintain the proper alignment of the commissure and prevent anterior glottic webs. In general, however, if a robust repair of mucosa and full reduction and stabilization of the laryngeal fracture can be achieved, it is preferable to avoid the use of stents given their potential complications. These complications include infection, granulation tissue and scar formation, and pressure necrosis, which is usually caused by using stents that are too large for the airway. Scarring from stents may lead to stenosis and impaired vocal cord mobility. There is a large variety of hollow and molded stents that vary in size, shape and material. The main classes of stents used are silicone, metal, and hybrid. Stent choice remains controversial and is usually surgeon-dependent, however silicone stents are generally preferred. On average, stents are usually left in place for 2 weeks and bronchoscopically removed in the operating room (3) (Table 3).
Full table
Penetrating wounds
Small tracheal wounds where there has been no loss of tissue and where the tracheal edges are well apposed can be treated non-operatively by temporary orotracheal or nasotracheal intubation. The cuff of the endotracheal tube should be inflated below the wound to prevent leakage of air into the subcutaneous and mediastinal spaces, thereby decreasing contamination of these areas. Small tracheal wounds usually seal spontaneously within 48 hours.
Any hemodynamically unstable patient who presents with a penetrating neck wound should undergo emergent neck exploration in the operating room. After securing the airway, laryngoscopic and bronchoscopic evaluation should be undertaken. Repair of any injuries should only be attempted after the airway is secure. The esophagus and hypopharynx should also be systematically evaluated for concurrent injuries by pharyngoscopy and esophagoscopy.
Tracheal transection
These injuries are usually fatal and patients will rarely survive to present to the emergency ward. In cases where the cervical trachea is completely transected, a transverse incision is made and an endotracheal tube is inserted into the distal trachea. The entire anterior chest should be prepared and draped into the operative field so that a median sternotomy can be performed if needed. Devitalized tracheal tissue and ragged edges should be debrided, however care must be taken to conserve as much remaining tracheal tissue as possible. Repair of the trachea is performed in an end-to-end interrupted fashion. Absorbable 4-0 sutures are placed through all tracheal layers, at an interval distance of 3 to 4 mm. Care should be taken to preserve the blood supply, which runs along both lateral aspects of the trachea, to prevent ischemia, which would impair healing of the repair site and promote stricture development. Internal stents are not necessary. At the end of the operation, a stay-suture is placed between the patient’s chin and chest to prevent neck extension and disruption of the repair. This stitch is removed after the anastomosis has healed and been surveilled by flexible bronchoscopy, usually on post-operative day seven (7).
Intrathoracic tracheal injuries are approached via a right posterolateral thoracotomy incision. Injuries to the posterior membranous portion of the trachea are also repaired through this approach and are primarily repaired and then buttressed with an intercostal muscle pedicle flap (Figure 5).
Mixed injuries
If both the trachea and esophagus have been injured, they should each be repaired primarily (Figure 6). The esophagus must be repaired in two layers. A flap of muscle, parietal pleura, or pericardium, as available, should be interposed between the two repair sites to promote healing and prevent the development of a tracheoesophageal fistula. In patients who have injuries to both the thoracic trachea and the esophagus with mediastinal contamination, the trachea should be primarily repaired and a cervical spit fistula should be constructed for esophageal diversion, with concurrent placement of a gastrostomy or jejunostomy feeding tube. The esophagus should be reconstructed several weeks later, after the tracheal repair has fully healed (11).
Higher mortality rates are seen in patients who have an associated vascular injury. Patients who sustain penetrating injury to the lower trachea are rarely salvageable due to associated lethal injuries to the heart or great vessels.
Complications
Delayed management of tracheal injury may result in a reduction in voice quality and changes in voice are commonly seen especially in patients who undergo extensive reconstructive procedures of the larynx. Twenty-one percent of patients who underwent surgical repair of the larynx for trauma had post-operative voice changes. Long-term speech therapy is therefore imperative in the rehabilitation of these patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Bacha E, Mathisen DJ, Grillo HC. Airway trauma. In: Westaby S, Odell JA. editors. Cardiothoracic Trauma. 1 ed. London: Oxford University Press, 1999.
- Classics in thoracic surgery: Total pneumonectomy. Rudolf Nissen, M.D. Ann Thorac Surg 1980;29:390-4. [PubMed]
- Lee WT, Eliashar R, Eliachar I. Acute external laryngotracheal trauma: diagnosis and management. Ear Nose Throat J 2006;85:179-84. [PubMed]
- Kelly JP, Webb WR, Moulder PV, et al. Management of airway trauma. II: Combined injuries of the trachea and esophagus. Ann Thorac Surg 1987;43:160-3. [Crossref] [PubMed]
- Kiser AC, O'Brien SM, Detterbeck FC. Blunt tracheobronchial injuries: treatment and outcomes. Ann Thorac Surg 2001;71:2059-65. [Crossref] [PubMed]
- Gluckman JL, Mangal AK. Laryngeal trauma. In: Paparella MM, Shumrick DA, Gluckman JL, et al. editors. Otolarngology, Vol III: Head and neck. Philadelphia: Saunders, 1991:2231.
- Mathisen DJ, Grillo H. Laryngotracheal trauma. Ann Thorac Surg 1987;43:254-62. [Crossref] [PubMed]
- Schaefer SD. The acute management of external laryngeal trauma. A 27-year experience. Arch Otolaryngol Head Neck Surg 1992;118:598-604. [Crossref] [PubMed]
- Ramchand T, Choudhry OJ, Shukla PA, et al. Management of hyoid bone fractures: a systematic review. Otolaryngol Head Neck Surg 2012;147:204-8. [Crossref] [PubMed]
- Sniezek JC, Thomas RW. Laryngeal Trauma. In: Resident Manual of Trauma to the Face, Head and Neck. 1 ed. American Academy of Otolaryngology, 2012.
- Symbas PN, Hatcher CR Jr, Boehm GA. Acute penetrating tracheal trauma. Ann Thorac Surg 1976;22:473-7. [Crossref] [PubMed]