Long-term outcomes and prosthesis performance after transcatheter aortic valve replacement: results of self-expandable and balloon-expandable transcatheter heart valves
Abstract
Background: Data on transcatheter aortic valve replacement (TAVR) long-term clinical outcomes and hemodynamic performance of the self-expandable CoreValve (CV) and the balloon-expandable Edwards SAPIEN XT (ES) (Edwards Lifesciences, Irvine, California, USA) transcatheter heart valves (THV) are limited. Therefore, this study aimed to compare long-term clinical outcome data and hemodynamic performance of TAVR with either CV or ES.
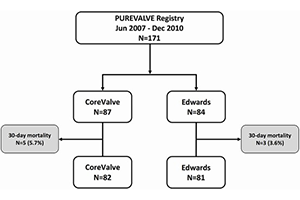
Methods: We reviewed prospectively collected data of 171 patients treated with TAVR for severe aortic stenosis (AS) at our center between June 2007 and December 2010, with last follow-up contact in 2016.
Results: Out of 171 patients treated with TAVR at our Institution, 87 received a CV and 84 an ES THV. Mean age was 81 [78–85] years, and mean Society of Thoracic Surgeons (STS) score was 7.5% [4.5–13.9%]. Hemodynamic success by Valve Academic Research Consortium (VARC) definition was 97.1%. Mean trans-prosthetic gradient remained low and stable during follow-up in both groups (at 5-year 9.2±6.4 versus 12.7±5.1 mmHg, P=0.10). Late prosthesis failure occurred in 4 cases (2.4%). Thirty-day mortality was 4.7%, and estimated survival rates by Kaplan-Meyer after 1, 5 and 8 years were 87.6%, 44.9%, and 24.5%, respectively, without difference between THV groups. Rates of cardiovascular death, stroke, myocardial infarction (MI) and congestive heart failure (CHF) were also similar with CV and ES at long-term follow-up. History of CHF, pre-existent severe mitral regurgitation, paravalvular leak grade ≥2+, and chronic obstructive pulmonary disease were independent predictors of late mortality at multivariate analysis.
Conclusions: Clinical and hemodynamic outcomes of patients treated by self-expandable CV or balloon-expandable ES THV were favorable and similar throughout long-term follow-up, with a rate of prosthesis failure of less than 3%.
Cover