Barrett’s esophagus: best practices for treatment and post-treatment surveillance
Abstract
Barrett’s esophagus (BE) is a premalignant condition that increases the risk of esophageal adenocarcinoma (EAC). Significantly more common in the Western world, risk factors include increased age, male sex, white race, gastro-esophageal reflux disease (GERD), central obesity, and cigarette smoking. The rates of progression to cancer depend on the grade of Barrett’s dysplasia. Screening for BE is recommended in patients with GERD and additional risk factors. Endoscopic surveillance of patients with BE likely improves overall outcomes. Advanced endoscopic imaging can help increase the efficiency of current endoscopic surveillance. Endoscopic therapy is safe and effective for the treatment of dysplastic BE and intramucosal EAC, but ongoing surveillance following treatment is necessary. This review will cover screening, surveillance, advanced imaging, chemoprevention, endoscopic treatment, and post-treatment surveillance of BE.
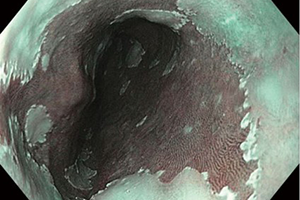
Cover