A meta-analysis of robotic vs. conventional mitral valve surgery
Introduction
Over the past few decades, minimally invasive surgery has transformed the landscape of cardiothoracic surgery in a wide range of procedures (1-3). Mitral valve surgery has traditionally been performed through a conventional sternotomy approach. However, a number of studies have demonstrated that comparable repair techniques can be performed in selected patients through a minimally invasive right mini-thoracotomy approach with potentially superior perioperative outcomes (4,5). More recently, robotic surgery involving telemanipulation systems has been developed to enable surgeons to perform mitral valve surgery with increased degrees of movement and improved vision.
Despite technological improvements in miniature instrumentation and development of operative techniques through increased experience, the extent of benefits derived from robotic surgery in patients with mitral valve disease remains uncertain. Currently, robotic mitral valve surgery remains limited to specialized centers for patients with isolated mitral valve pathology. To systematically appraise the available evidence, the present study aimed to identify all relevant studies on mitral valve surgery to compare the outcomes of robotic vs. conventional approaches. Primary endpoints included mortality, stroke and re-operation for bleeding. Secondary endpoints included length of hospitalization, duration of intensive care unit (ICU) stay, cross-clamp time and cardiopulmonary bypass time. Echocardiographic outcomes before and after robotic or conventional surgery were also assessed. This study represents the first meta-analysis of robotic vs. conventional mitral valve surgery.
Methods
Literature search strategy
Electronic searches were performed using Cochrane Database of Systematic Reviews, ACP Journal Club, Database of Abstracts of Reviews of Effects, Cochrane Central Register of Controlled Trials, Cochrane Methodology Register, Heath Technology Assessment, NHS Economic Evaluation Database, Embase and Ovid Medline from 1995 to July 2013. To achieve the maximum sensitivity of the search strategy and identify all studies, we combined the terms “mini*” or “thoraco*” or “video*” or “robot*” or “laparoscop*” or “endoscop*” or “port-access” or “port access” or “partial sternotomy” or “keyhole” and “mitral*” or “Barlow*” as either keywords or MeSH terms. The reference lists of all retrieved articles were reviewed for further identification of potentially relevant studies. All relevant articles identified were assessed with application of the selection criteria.
Selection criteria
Eligible comparative studies for the present meta-analysis included those in which patients with mitral valve disease underwent surgery either through the conventional sternotomy or robotic approach. When institutions reported duplicated trials with accumulating numbers of patients or increased lengths of follow-up, only the most complete studies were included. All publications were limited to human subjects and English language. Abstracts, case studies, conference presentations, editorials and letters were excluded.
Data extraction and critical appraisal
All data were extracted from article texts, tables and figures. When insufficient data were available from publications, corresponding authors were contacted to provide additional records. Three investigators (S. G., T. A. N., and D. C.) independently reviewed each retrieved article. Discrepancies between the reviewers were resolved by discussion and consensus. The final results were reviewed by the senior investigators (C. C. and T. D. Y.).
Statistical analysis
Meta-analysis was performed by combining the results of reported incidences of mortality, stroke, re-operation for bleeding and durations of hospitalization, ICU stay, cross-clamp time and cardiopulmonary bypass time when comparable outcomes were available. The relative risk (RR) was used as a summary statistic and the random effects model was tested, as it was assumed there were variations between studies and the calculated ratios had a more conservative value (6). χ2 tests were used to study heterogeneity between trials. I2 statistic was used to estimate the percentage of total variation across studies, due to heterogeneity rather than chance. An I2 value of greater than 50% was considered substantial heterogeneity. If there was substantial heterogeneity, the possible clinical and methodological reasons for this were explored qualitatively. All P values were two-sided. All statistical analysis was conducted with Review Manager Version 5.1.2 (Cochrane Collaboration, Software Update, Oxford, United Kingdom).
Results
Quantity and quality of trials
A total of 4,968 references were identified through the nine electronic database searches. After exclusion of duplicate or irrelevant references, 66 potentially relevant articles were retrieved for more detailed evaluation. After applying the selection criteria, six comparative studies remained for assessment. Manual search of the reference lists did not identify any additional relevant studies. A summary of the search strategy is presented in Figure 1. All of selected studies were retrospective observational studies, as summarized in Table 1 (7-12). In these six studies, 1,650 patients who underwent mitral valve surgery were compared, including 960 patients who underwent the robotic approach and 690 patients who underwent the conventional sternotomy approach.

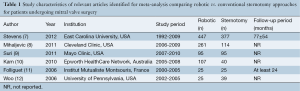
Full table
Patient characteristics
Four out of the six selected studies reported that all patients in both the robotic and conventional groups had isolated myxomatous valve pathology (8-11). One study did not provide sufficient pathological details (12) and another study included a significant proportion of patients who had other mitral valve pathologies (7). Two retrospective studies matched patient cohorts according to prognostic factors (8,9). However, patients in the robotic group tended to be younger, with fewer incidences of diabetes and hypertension. In addition, there was a trend towards better functional status for patients included in the robotic surgical arm. A summary of these patient baseline characteristics is presented in Tables 2,3.
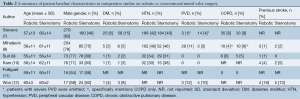
Full table
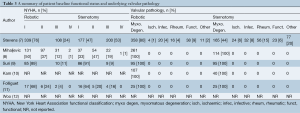
Full table
Surgical techniques
All of the reported robotic mitral valve surgeries were performed through two or three ports and a 3-5 cm right mini-thoracotomy using the da Vinci® Surgical System (Intuitive Surgical Inc., Sunnyvale, CA, USA). Three out of the six studies reported using the endoaortic balloon occlusion device for patients who underwent robotic surgery (7,8,12). Concomitant surgical procedures such as atrial fibrillation ablation and atrial septal defect closures were reported in three studies (7-9). A summary of procedural details, including the cardioplegia strategy and repair techniques, is presented in Table 4.
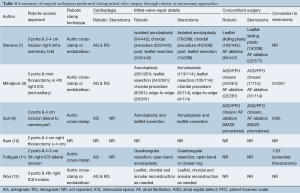
Full table
Assessment of primary endpoints
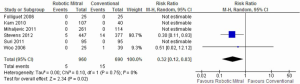
Mortality
Although all six selected studies reported the incidences of all-cause perioperative mortality, only two studies reported deaths that occurred. From the available data, patients who underwent mitral surgery through the robotic approach had a significantly lower incidence of mortality compared to the conventional sternotomy approach [0.5% vs. 2.2%; RR, 0.32; 95% confidence interval (CI), 0.12-0.83; P=0.02; I2=0%]. These results are presented in Figure 2.
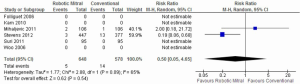
Stroke
Three studies reported on the incidences of perioperative stroke, and two studies recorded events. From the available data, there was no significant difference between the robotic vs. conventional approaches (0.8% vs. 2.4%; RR, 0.50; 95% CI, 0.05-4.65; P=0.54; I2=65%). These results are presented in Figure 3.
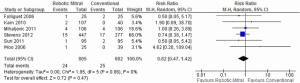
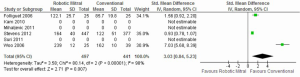
Re-operation
Re-operation for bleeding was reported in all studies, and there were no significant differences between the robotic vs. conventional approaches (3.0% vs. 3.7%; RR, 0.82; 95% CI, 0.47-1.42; P=0.47; I2=0%). These results are presented in Figure 4.
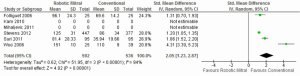
Assessment of secondary endpoints
Meta-analysis identified a significantly longer duration of cross-clamp time [standardized mean difference (SMD), 2.05; 95% CI, 1.23-2.87; P<0.00001; I2=94%] and cardiopulmonary bypass time (SMD, 3.03; 95% CI, 0.84-5.23; P=0.007; I2=98%) for patients who underwent robotic surgery vs. conventional approach. These results are presented in Figures 5,6, respectively. The lengths of hospitalization (SMD, –1.07; 95% CI, –2.83-0.70; P=0.24; I2=96%) and ICU stay (SMD, –1.58; 95% CI, –3.45-0.29; P=0.10; I2=97%) were not significantly different between the two approaches.
Sensitivity analysis
Stevens et al. reported a number of significant differences between the baseline patient characteristics of the robotic and conventional treatment groups (7). In addition, unlike other studies included in the present meta-analysis, a significant proportion of patients had ischaemic, rheumatic, infective or functional mitral valve pathology. Hence, a sensitivity analysis was performed by excluding data from this study. By doing so, the perioperative mortality outcome was no longer statistically significant between the robotic vs. conventional treatment arms, as only one other study reported any incidence of deaths.
Echocardiography outcomes
Available echocardiographic findings were categorized into predefined severities of mitral regurgitation. Preoperatively, 443/502 patients undergoing robotic surgery had severe regurgitation and 59/502 had moderate regurgitation. The respective figures were 264/297 and 33/297 for patients undergoing conventional sternotomy. Postoperatively, 4/346 patients who underwent robotic surgery had moderate regurgitation, 24/346 had mild regurgitation and 318/346 had trivial or no residual regurgitation. The corresponding figures were 4/285, 18/285 and 263/285 for patients who underwent conventional sternotomy. A summary of these echocardiographic findings before and after surgery is presented in Figure 7A,B.

Discussion
Mitral valve surgery through the robotic approach enables the surgeon minimal access and 7 degrees of freedom of movement, with additional benefits of three-dimensional visualization, tremor minimization and avoidance of the fulcrum effect associated with long-shafted endoscopic instruments. Proponents of robotic mitral surgery propose that similar surgical repairs can be performed through the minimally invasive approach as conventional sternotomy, with potential benefits of reduced trauma and associated advantages of reduced blood product requirement and shorter hospitalization (12). Expert robotic surgeons from specialized institutions have demonstrated the feasibility of performing complicated mitral repair techniques through the robotic approach without compromising surgical outcomes (7). Recently, Nifong et al. reported excellent results in a group of 540 patients who underwent robotic mitral valve repairs including concomitant biatrial cryoablation procedure (13).
To systematically evaluate the outcomes of robotic vs. conventional mitral surgery, the present meta-analysis identified all comparative studies in the existing literature and found that robotic mitral valve surgery was associated with a statistically significant survival benefit over conventional surgery. Perioperatively, there were no significant differences in regards to the incidences of stroke or re-operation for bleeding. Cross-clamp and cardiopulmonary bypass times were significantly longer for robotic surgery, but the durations of hospitalization and ICU stay were not statistically different between the two surgical techniques.
A number of limitations to our study should be acknowledged and the results should be interpreted with caution. Firstly, our systematic review of the current literature has demonstrated that the quantity and quality of the existing evidence for robotic vs. conventional surgery is very limited. All six studies included in the meta-analysis were retrospective case-series reports with differences between the robotic and conventional patient cohorts. Without randomization, surgical outcomes may reflect the patient characteristics rather than the surgical intervention. However, attempts were made in two studies to match patients according to propensity scores to minimize selection bias (8,9). The large study by Stevens et al. reported a heterogenous cohort of patients with various mitral valve pathologies and unbalanced patient baseline characteristics. When data from this study was excluded from analysis, the mortality difference between the two surgical techniques was no longer significant. Secondly, as with any novel surgical or medical intervention, there is the possibility for publication bias, with potentially more favorable outcomes being reported from large volume expert centers that may not be representative of all institutions. Finally, significant heterogeneity was detected for the analysis of stroke and secondary outcomes such as cross-clamp time, cardiopulmonary bypass duration and length of hospitalization. This may reflect the limited number of studies and different surgical techniques and clinical practices, respectively.
In conclusion, the present meta-analysis identified a statistical survival benefit for robotic mitral valve surgery vs. the conventional sternotomy approach. However, this was largely a reflection of the heterogenous patient cohort between the two treatment arms within the identified retrospective studies. Without randomization and adequate patient matching, the existing evidence for robotic surgery is not robust, and limited conclusions can be drawn from the current literature. However, it has been demonstrated that robotic mitral valve surgery can be feasibly performed by expert surgeons for selected patients. These centers have recognized that a successful robotic surgical program is dependent on the development of a highly specialized and well-trained team including anesthesiologists, perfusionists, operating room staff, and surgeons (14). In addition, they believe that surgical units must be able to maintain a sufficient volume of referrals to attain and maintain safety. As there is currently limited robust clinical data on the surgical outcomes of robotic mitral valve surgery, this novel procedure should be limited to specialized centers that fulfil the above criteria. Ultimately, surgical outcomes of mitral valve surgery will be dependent on choosing the right procedure by the right surgeon for the right patient, rather than by the length of the skin incision (15).
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Cao C, Ang SC, Indraratna P, et al. Systematic review and meta-analysis of transcatheter aortic valve implantation versus surgical aortic valve replacement for severe aortic stenosis. Ann Cardiothorac Surg 2013;2:10-23. [PubMed]
- Cao C, Manganas C, Ang SC, et al. A systematic review and meta-analysis on pulmonary resections by robotic video-assisted thoracic surgery. Ann Cardiothorac Surg 2012;1:3-10. [PubMed]
- Cao C, Manganas C, Ang SC, et al. A meta-analysis of unmatched and matched patients comparing video-assisted thoracoscopic lobectomy and conventional open lobectomy. Ann Cardiothorac Surg 2012;1:16-23. [PubMed]
- Speziale G, Nasso G, Esposito G, et al. Results of mitral valve repair for Barlow disease (bileaflet prolapse) via right minithoracotomy versus conventional median sternotomy: a randomized trial. J Thorac Cardiovasc Surg 2011;142:77-83. [PubMed]
- Ryan WH, Brinkman WT, Dewey TM, et al. Mitral valve surgery: comparison of outcomes in matched sternotomy and port access groups. J Heart Valve Dis 2010;19:51-8; discussion 59. [PubMed]
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. [PubMed]
- Stevens LM, Rodriguez E, Lehr EJ, et al. Impact of timing and surgical approach on outcomes after mitral valve regurgitation operations. Ann Thorac Surg 2012;93:1462-8. [PubMed]
- Mihaljevic T, Jarrett CM, Gillinov AM, et al. Robotic repair of posterior mitral valve prolapse versus conventional approaches: potential realized. J Thorac Cardiovasc Surg 2011;141:72-80.e1-4.
- Suri RM, Burkhart HM, Daly RC, et al. Robotic mitral valve repair for all prolapse subsets using techniques identical to open valvuloplasty: establishing the benchmark against which percutaneous interventions should be judged. J Thorac Cardiovasc Surg 2011;142:970-9. [PubMed]
- Kam JK, Cooray SD, Kam JK, et al. A cost-analysis study of robotic versus conventional mitral valve repair. Heart Lung Circ 2010;19:413-8. [PubMed]
- Folliguet T, Vanhuyse F, Constantino X, et al. Mitral valve repair robotic versus sternotomy. Eur J Cardiothorac Surg 2006;29:362-6. [PubMed]
- Woo YJ, Nacke EA. Robotic minimally invasive mitral valve reconstruction yields less blood product transfusion and shorter length of stay. Surgery 2006;140:263-7. [PubMed]
- Nifong LW, Rodriguez E, Chitwood WR Jr. 540 consecutive robotic mitral valve repairs including concomitant atrial fibrillation cryoablation. Ann Thorac Surg 2012;94:38-42; discussion 43. [PubMed]
- Bush B, Nifong LW, Chitwood WR Jr. Robotics in cardiac surgery: past, present, and future. Rambam Maimonides Med J 2013;4:e0017. [PubMed]
- Mihaljevic T, Gillinov M. Invited commentary. Ann Thorac Surg 2012;93:1468. [PubMed]





